Introduction & Background
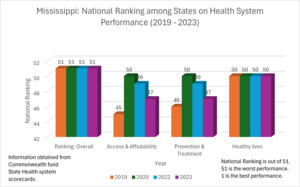
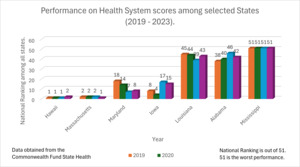
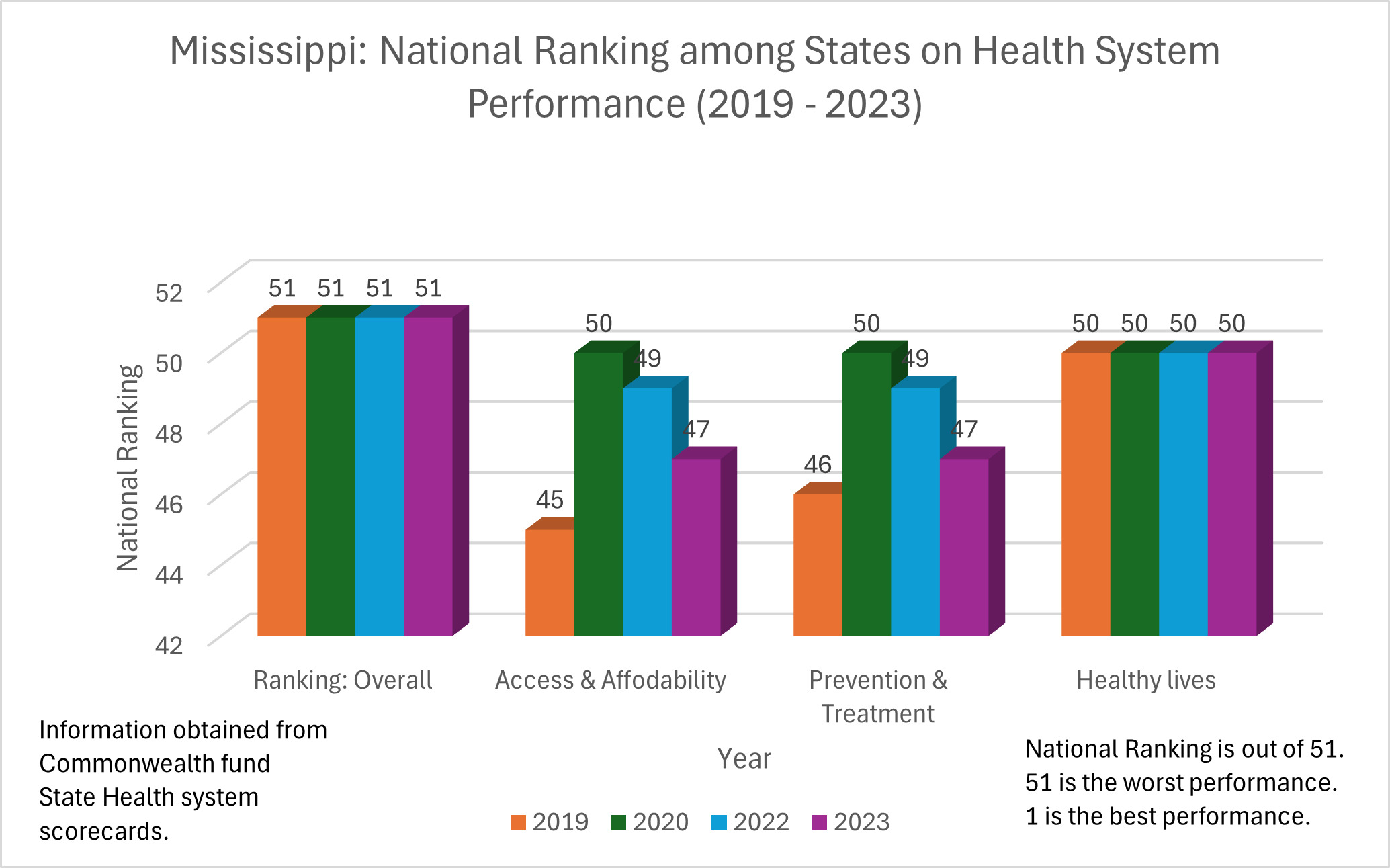
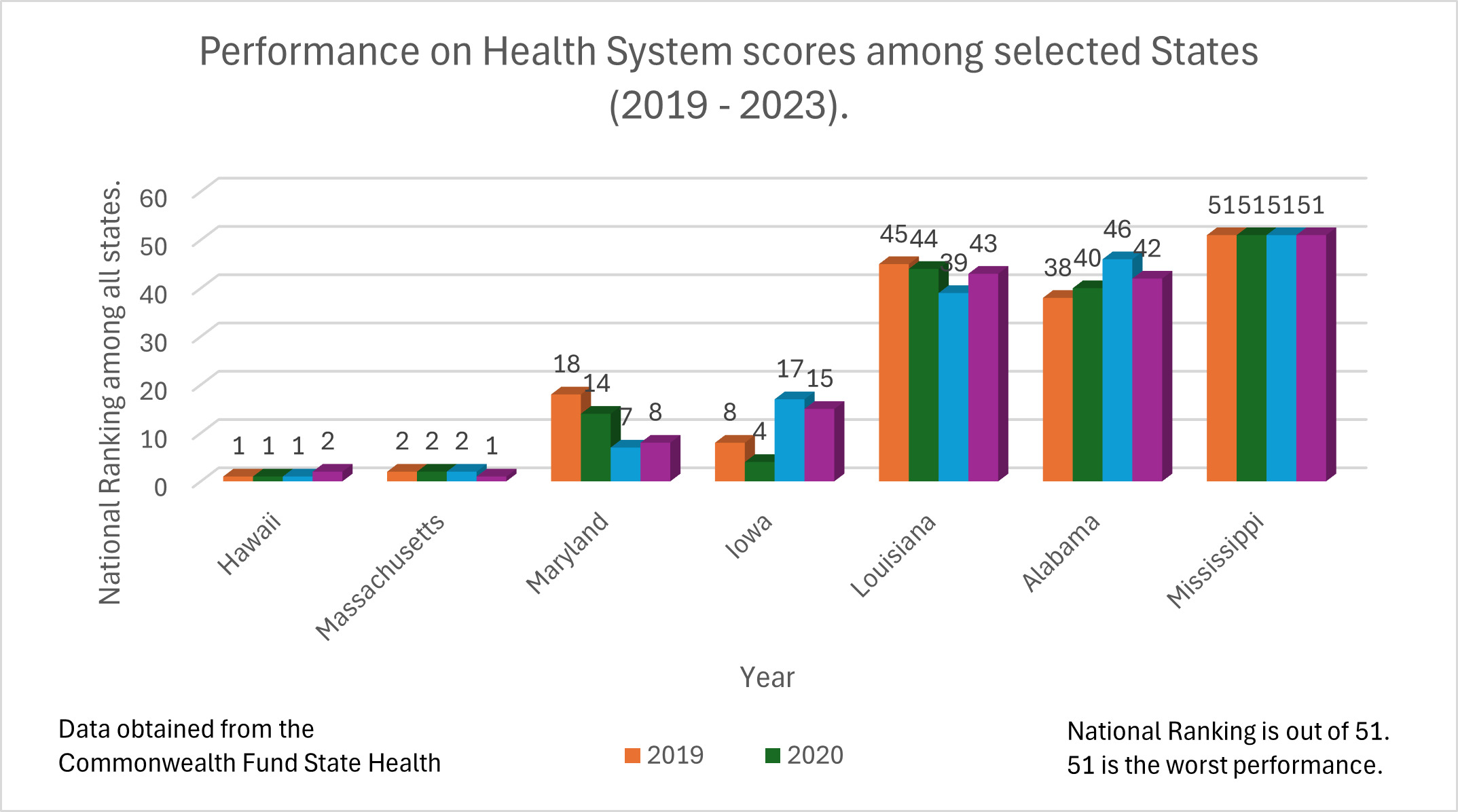
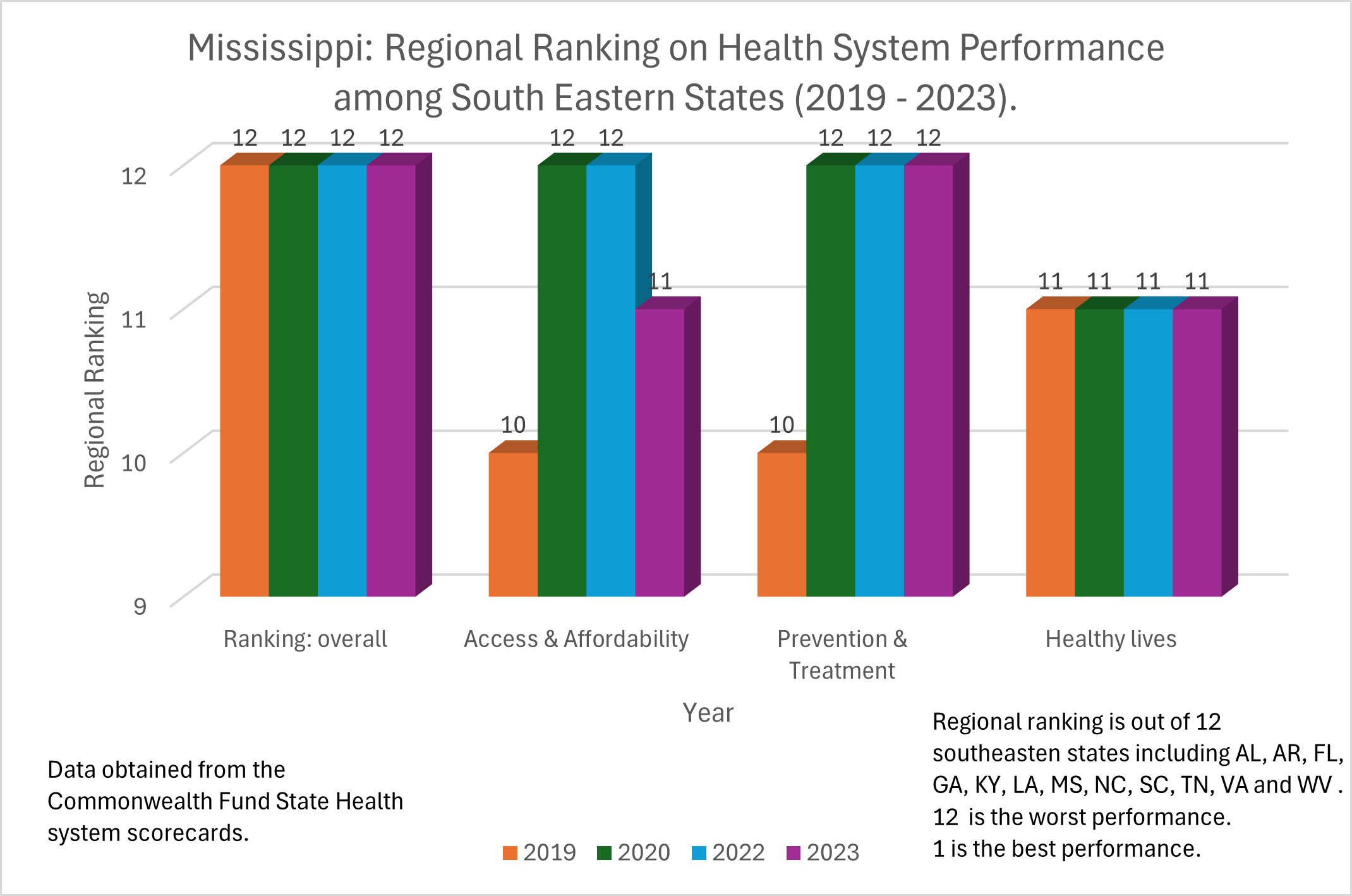
Mississippi, known for its geography, music, and Southern hospitality, also boasts a high rank in the natural environment, with great scores in air and water quality.1 However, this contrast is stark when we consider that Mississippi, with a population of about 2.94 million people, has the lowest per-capita income of any state in the country and the highest poverty rate.2,3 Despite leading in preschool immunization for several years4–7 and still ranking among the top states in polio vaccination,8 it also holds the unfortunate title of the unhealthiest population in the nation.9 Furthermore, it continues to maintain the worst-performing health care system in the United States.10–13 Table 1 and Figure I illustrate these rankings among the states based on the annual report of the Commonwealth Funds from 2019 to 2023 (there was no report for 2021 due to COVID-19). Table 2 and Figure 2 provide a comparative view of the performance among a few selected states (Hawaii, Massachusetts, Maryland, Iowa, Louisiana, Alabama, and Mississippi for 2019, 2020, 2022, and 2023).
If the states in the USA were countries, Mississippi in 2016 would tie with Kuwait as 76th in the world,14 while Hawaii would rank 20th in the world. In 2019, Mississippi would have ranked 80th, along with Malaysia and Belarus.15 In Mississippi, for every 100 babies born in 2019, three will not reach their 30th birthday, ten will not live to see 50, and 24 will pass away before turning 65. In contrast, in Hawaii, only 14 out of 100 will die before their 65th birthday.16 Of the years they live, Mississippi men and women spend about 9% and 12% of their adult lives, respectively, with a disability.17 The data is significantly worse for Mississippians who have systematically faced obstacles limiting the attainment of good health outcomes. Such obstacles include geographic location, socioeconomic status, ethnicity, and sexual orientation. Although these groups are disproportionately affected, health disparities limit the overall improvements in the quality of care and health status of the entire population.18
Data Sources and Ranking
The Commonwealth Fund is a non-profit, non-political organization that has produced reports comparing healthcare systems in high-income countries since 2004. The Commonwealth Fund aims to promote high-performing healthcare systems that produce better access, improved quality, and greater efficiency, especially for the most vulnerable in society.19,20 Reports on data, interactives, and benchmarking scorecards have been published annually for the various states in the USA for many years and reflect how well the healthcare system is working. All 50 states and the District of Columbia are assessed on a number of measures of access to health care, service use, cost, quality of care, health outcomes, and income-based health care disparities. In 2020, the assessment used 49 measures, which increased to 58 measures in 2023. An overall score ranks the different states based on performance on the various items, and a specific profile for each state is developed. Such rankings and reports require cautious interpretation since the various states differ in many ways.
There is a time lag due to the time required for the data to be completely recorded, collected, analyzed, and verified. Data from 2019 reflects 2017 status, 2020 reflects 2018 status, 2022 reflects 2020 status, and 2023 reflects 2021 status. There was no comparable data report for 2021 due to the effects of the COVID-19 pandemic.
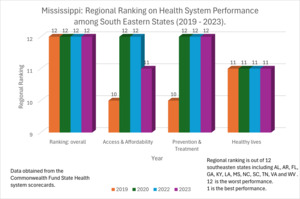
Data from 2019 to 2023 all rank Mississippi 51 out of 51, reflecting the worst performing health care system for any state in the USA. When viewed among the Southeastern states (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia), Mississippi ranks 12 out of 12. Table 3 and Figure 3 show the sub-ranking for the state among its Southeastern peers. Access and affordability in Mississippi ranked best, followed by prevention and treatment in 2019.
USNews1 ranked the state 50th among the 50 states using 71 metrics across 8 categories based on the average of 3 years of data from national surveys. The ranking in the subcategories (public health 46, health care quality 48, and health care access 49) was similar to those on the Commonwealth Fund metrics.
Discussion
Health indicators are dynamic summary estimates that track the performance of a health system or a particular aspect of health status. These indicators are useful for measuring the outcomes of health care inventions or interventions. They provide feedback on decision-making and provide clues to future trends.21,22 For instance, the Infant Mortality Rate (IMR) provides information on infant and maternal health as well as the overall health of the society and is very sensitive to general structural factors like socioeconomic development and basic living conditions.23,24
Many factors contribute to this state of health care, and improving the status quo requires dialogue and collaboration that will involve the policymakers, health care workers, community leaders, and local stakeholders in walking the difficult line of prioritizing resource allocation and balancing critical priorities, one of which is health care. The choices are not usually all-or-none, and these choices are usually not made in isolation. While there are several factors operating at the macrostructural levels (like state policies) and individual-proximal levels (for instance, health behaviors) to determine health and mortality, the macrostructural factors are the most important and exert a more substantial influence on the other levels. Policies and the political choices underlying them are “the causes of the causes of the causes” of the observed geographic inequities in health.15,25
The data and rankings for Mississippi portray a perennial picture that physicians, policymakers, and the lay public need to recognize not only for what it shows but also for what it portends. As one crisis follows another, it is relatively easy to relegate this chronic, recurrent last-place position to the background. Are we doing more harm by doing nothing (malignant neglect) or offering inconsequential solutions?26,27 Complacency engenders a false sense of security. It entails being contented or comfortable with the status quo, unaware of the potential hazards.
Public health information can sound abstract and not reflect to the lay public the gravity of the data it presents. For instance, a decline in life expectancy from 79 years to 78 years may appear to be just a decrease by only one year, but it really means that thousands of premature deaths will have to happen for that decrease to occur. Galea et al.28 estimated that the United States would have avoided 245,000 deaths in one year alone if the adult population with low education levels experienced the death rates of those with higher education levels.
While the Infant Mortality Rate in Mississippi is the worst in the nation, the state continues to maintain one of the highest vaccination rates in the nation. It has shown relative improvements in the ranking for diabetes and obesity.29 Improving the health system and the population’s health will also provide benefits for other sectors like education, work, economic opportunities, family, social mobility, and sustainable development. Health is wealth and bears heavily on people’s well-being. A healthy population is a prerequisite for a thriving economy and sustainable development.
Acknowledgement
The authors report no conflict of interest.