Case Presentation
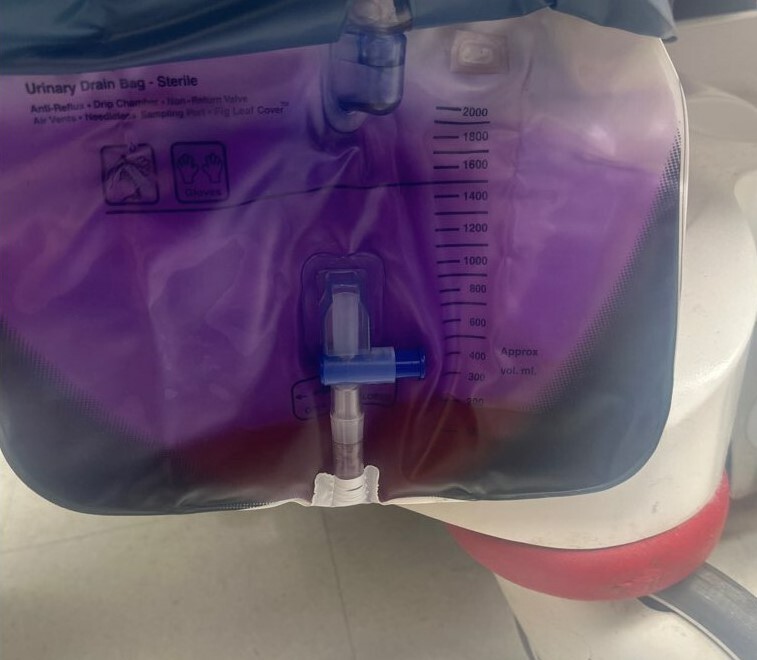
A 73-year-old female with a history of hypertension, type 2 diabetes mellitus, paroxysmal atrial fibrillation, and stroke presented to the emergency department (ED) for decreased urine output and purple discoloration of urine and foley bag for an unknown amount of time. Family also reported constipation and occasional lower abdominal discomfort. She had an indwelling catheter secondary to urinary retention after a stroke 6 months ago, and it was last replaced 3 months prior to her ED presentation. Patient was not on medications known to alter urine color. Her vitals on arrival were normal except for a heart rate of 110 bpm. She had tenderness to palpation in her lower abdomen, orange-brown urine in foley bag, and purple discoloration of bag, tubing, and urine in tubing (Figures 1, 2 and 3). Labs were significant for creatinine 2.72 mg/dL, BUN 51.4 mg/dL, and WBC 13,300/cm2. Urine prior to foley catheter replacement had 500 leukocytes/uL, few bacteria/HPF, >100 WBC/HPF, 10 RBC/HPF, and a pH of 7.5. Urine after catheter exchange had 250 leukocytes/uL, moderate bacteria/HPF, 63 WBC/HPF, 4 RBC/HPF and a pH of 8.5.
Discussion
The patient was diagnosed with a urinary tract infection (UTI) and purple urine bag syndrome (PUBS). She was started on empiric vancomycin and ceftriaxone. The culture of her urine from her existing urine bag grew out >100,000 Citrobacter freundii complex and an insignificant colony count of gram-negative bacilli while the culture of urine after catheter and bag replacement grew out >100,000 Escherichia coli. She was transitioned to just ceftriaxone based on urine culture and sensitivity results. Patient’s acute kidney injury and urine color improved with IV crystalloids and antibiotics, and she was discharged home on hospital day 3 on oral cefixime.
PUBS is characterized by purple discoloration of the urine and/or bag. The urine itself can be described as purple, orange, or brown.1 PUBS was first described in 1978 by Barlow et al., but it still remains an uncommon phenomenon.2 It is benign and can be seen with ingestion of medications, such as methylene blue and hydroxycobalamin, and with underlying pathology such as a UTI.3 The urinary bacterial organisms typically implicated are Escherichia coli, Klebsiella pneumoniae, Proteus species, Providencia species, Morganella morganii, Pseudomonas aeruginosa, Enterobacter species, and Citrobacter species.1,4–6
PUBS is a manifestation of intestinal tryptophan metabolism into indole which is conjugated in the liver to form indoxyl sulfate (indican). Indoxyl sulfate is secreted into the urine and converted to indoxyl by bacterial sulfatases and phosphatases. Indoxyl is oxidized to indigo and indirubin, which are blue- and red-pigmented, respectively, and this is augmented by alkaline urine.1,4,6,7 The combination of these pigments can cause urine and/or foley bag to turn purple. Constipation, as seen in our patient, can cause overgrowth of bacteria that metabolize tryptophan.7 Other predisposing factors to PUBS include high urinary bacterial counts, female gender, advanced age, long-term catheterization, institutionalization, dementia, kidney disease, obesity, and type 2 diabetes mellitus.1,4,6,7 As discussed in the case presentation, our patient had many of the above predisposing risk factors for PUBS.
Healthcare professionals should recognize that PUBS in and of itself is benign, and that the presence of this condition typically indicates an underlying UTI in the presence of certain predisposing factors. Early recognition of such pathology and predisposing factors can lead to timely diagnosis and treatment which can lead to better patient outcomes.
Informed consent was obtained directly from the patient.