1. Introduction
Nasopalatine duct cysts are the most common non-odontogenic cyst of the oral cavity in the general population, but their incidence among pediatric populations is low. We present a case of a giant nasopalatine duct cyst in a 15-year-old male, which resulted in significant distortion of the sinonasal architecture.
2. Case Presentation
A 15-year-old boy was referred to our clinic by his otolaryngologist for a nasal mass. The patient had been experiencing symptoms of worsening nasal congestion for several months in addition to nasal mass expansion and resultant deformation of the shape of his face (Figure 1). There was no previous history of trauma to the face. The patient had no history of dental surgery or dental extractions but did have braces. Physical examination of the head and neck revealed upward displacement of the nose with widening at its base. A mass was present and filled the nasal cavity, resulting in complete obstruction of both nasal passages due to nasal floor elevation. A mild bulge was also noted in the anterior hard palate. Radiographic examination revealed a homogenous, non-enhancing soft-tissue density measuring 6.6 x 5.2 x 5.6 cm in the anterior inferior nasal cavity resulting in bony expansion and thinning of the ethmoid cavities. (Figure 2) The maxillary sinuses were bilaterally compressed and mostly opacified with leftward nasal septal deviation. A preliminary diagnosis of nasopalatine duct cyst was made based off these imaging and physical exam findings.
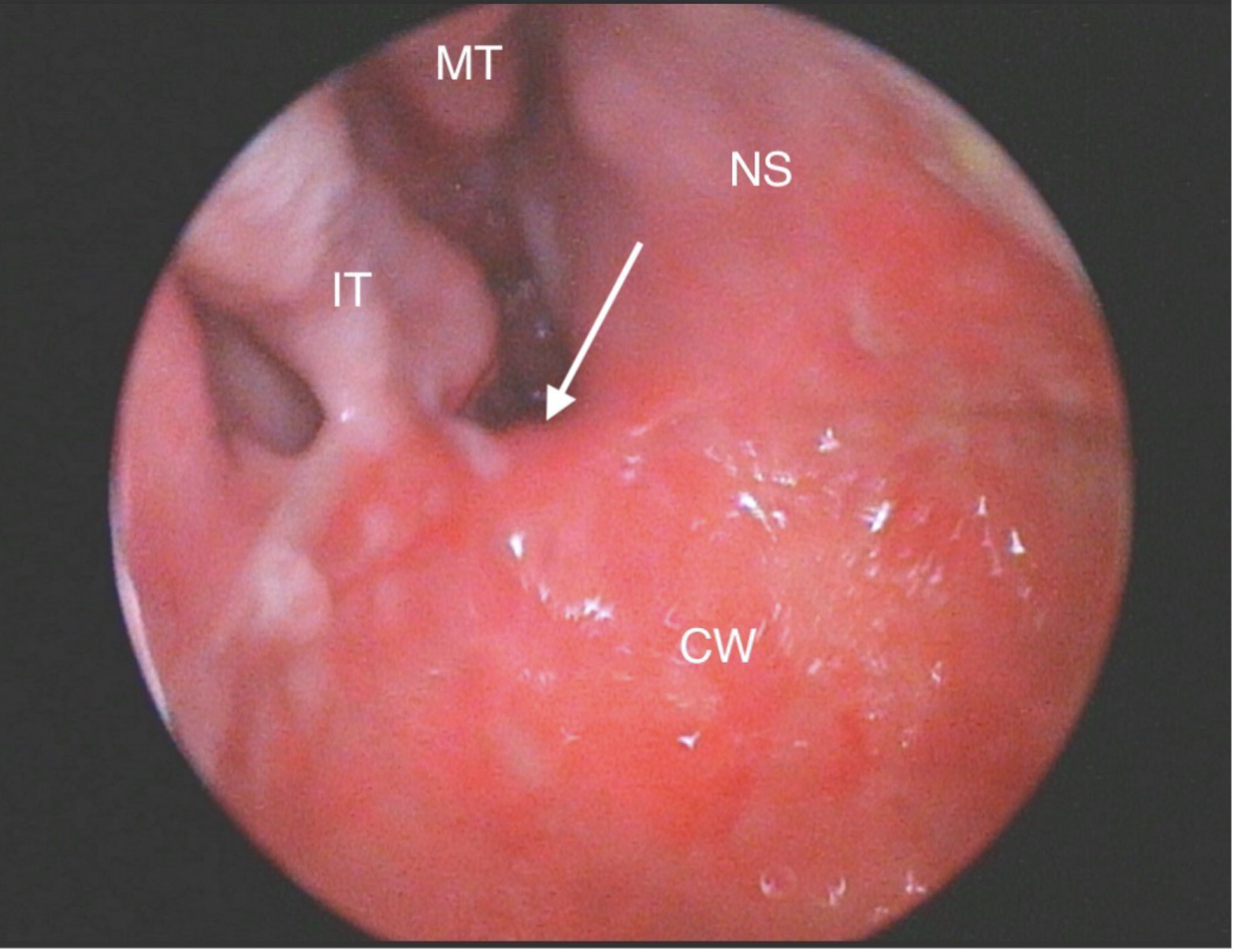
Recommendations were made for surgery, and endoscopic marsupialization of the cyst was performed under general anesthesia. Following marsupialization and removal of cyst contents, the bilateral nasal cavities were examined revealing severe leftward septal deviation as well as displacement of inferior and middle turbinates as previously noted on computed tomography scan. The decision was then made to perform limited functional endoscopic sinus surgery with bilateral maxillary antrostomy and anterior ethmoidectomy. A Doyle stent was placed on the left side and secured for two weeks.
Pathological examination revealed a benign developmental cyst lined by a combination of ciliated columnar and squamous epithelium consistent with nasopalatine duct cyst. The patient was seen in clinic 14 days later for stent removal and, despite some residual discomfort, the tissues were healing well. Upon follow-up examination at 4 and 8 months, the cavity size appeared to be shrinking, and the nasal bones were returning to their natural position (Figure 3).
3. Discussion
Nasopalatine duct cysts, i.e., incisive foramen cysts, represent the most common nonodontogenic cyst of the oral cavity, with an estimated prevalence of around 1% of the general population.1 Although the etiology of these cysts is uncertain, they are often believed to arise from proliferation of epithelial remnants of the nasopalatine duct, a structure formed during fetal development that connects the oral and nasal cavities near the incisive canal.1–3 While the nasopalatine duct typically degenerates, epithelial remnants may persist in the incisive canals of some individuals. Nasopalatine duct cysts most likely are the result of spontaneous cystic degradation of those remnants, though it has also been suggested that irritation, local trauma, or infections can cause this proliferation.1–3 Nasopalatine duct cysts may develop at any age, but they are most commonly reported in patients aged 40 to 60 years old. Though nasopalatine duct cysts are considered by many as developmental cysts, they rarely present within the first ten years of life and are more commonly found in males.1,2,4
Many nasopalatine duct cysts are asymptomatic and only diagnosed from routine radiographic examination.1,5 For lesions that are symptomatic, the most common presenting symptoms include anterior palate swelling, drainage, and pain (likely due to compression of adjacent structures).1,3 Differential diagnoses for physician consideration include enlarged nasopalatine duct, central giant cell granuloma, central incisor root cyst or other maxillary cysts, osteitis fistulizing in the palatine direction, or bucconasal and/or buccosinusal communication.3
Radiological examination of nasopalatine duct cysts typically demonstrates “well-circumscribed radiolucency in or near the midline of the anterior maxilla, between and apical to the central incisor teeth”.1 The lesion is most often round or oval and features a sclerotic border, though some cysts have an inverted pear or heart shape due to involvement of surrounding structures.1,5 The diameter of these lesions can vary, but most cysts have a diameter between 1.0 and 2.5 cm, with an average diameter of 1.5-1.7 cm.1
Histological presentation for nasopalatine duct cysts is varied, and epithelium type can range from stratified squamous epithelium (the most common presentation) to a combination of pseudostratified columnar epithelium, simple columnar epithelium, and simple cuboidal epithelium.2,5 While there is no association between type of epithelium and size of the cyst, there is an association between type of epithelium and positioning of the lesion.5 A lesion developing near the nasal cavity is more likely to exhibit features of the ciliated respiratory epithelium commonly found in that region. Conversely, a more inferior lesion location will typically result in a greater similarity to the squamous epithelium of the oral cavity.2–7 The cyst wall typically contains nerves, arteries, and veins, but it may also contain salivary gland parenchyma and cartilage. Mild to severe inflammatory response is often observed. The cystic capsule often contains blood vessels, nerves, mucous glands, and cholesterol crystals. Other capsule contents may include muscle, adipose tissue, reactional bone formation, melanin pigments, and daughter cysts. Inflammatory filtrate is often present.2
Treatment for nasopalatine duct cysts almost always includes surgical excision and curettage, with surgical approach (palatine, labial, combined palatine/labial) determined by lesion size and location.2,3,5 Surgical complications, although rare, may include damage to the floor of the nose, oronasal communication, fistula, possible damage to adjacent teeth, infections, hemorrhage, and parasthesia.2,8,9 Several recent case reports have demonstrated that more conservative surgery of large nasopalatine duct cysts with endoscopic marsupialization can offer rapid healing and low morbidity, and this case report adds to the literature supporting endoscopic marsupialization.10–13
4. Conclusion
Giant nasopalatine duct cysts are rare and can present significant treatment challenges. In this case of complete nasal obstruction and bilateral sinus ostial impingement, the patient was successfully managed with endoscopic marsupialization and sinus surgery.