Case presentation
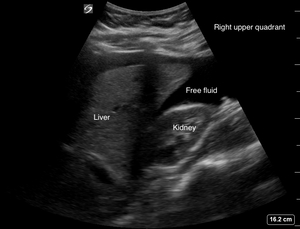
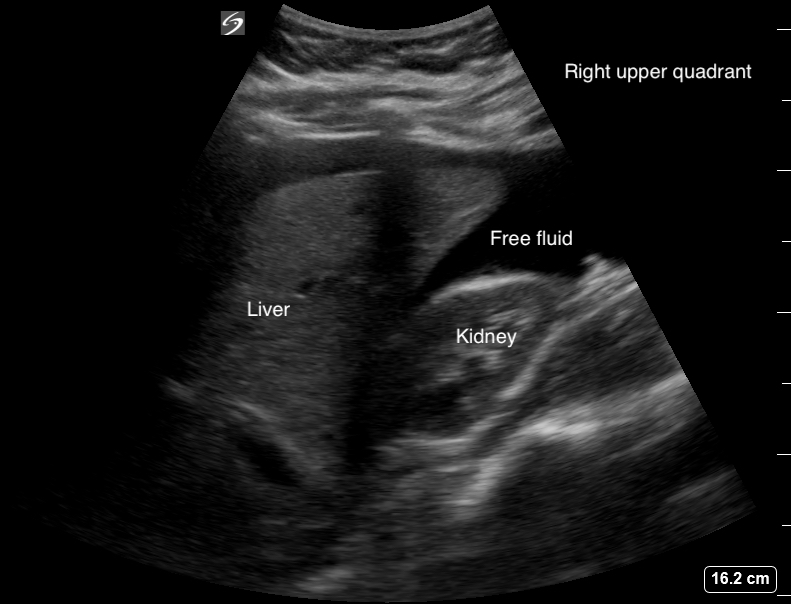
A 19-year-old female, gravida 1 para 0 at 7-weeks 3-days gestation by last menstrual period, consistent with recent (6-week 2-days) ultrasound, presented to the emergency department (ED) for evaluation after a syncopal episode with associated abdominal pain. She also noted intermittent vaginal bleeding over the previous week. She reports a normal intrauterine pregnancy (IUP), as determined by ultrasound, during a recent obstetrical workup for her pregnancy. Her vital signs on arrival were as follows: blood pressure 98/46 and heart rate 69 bpm, with a normal temperature, respiratory rate, and oxygen saturation. She was noted to be guarding on abdominal exam and had both tenderness to palpation and rebound tenderness. Her past medical history was significant for a diagnosis of chlamydia and bacterial vaginosis. A Focused Assessment with Sonography in Trauma (FAST) exam via point-of-care ultrasound (POCUS) was performed in the ED (Figures 1, 2 and 3).1
Images
Discussion
An intrauterine pregnancy with fetal cardiac activity was noted on ED POCUS. An extrauterine pregnancy could not be excluded. Due to a positive FAST scan (fluid in the RUQ), the findings and clinical presentation were concerning for a possible heterotopic pregnancy consisting of a viable IUP and a ruptured ectopic pregnancy. The Ob-Gyn team was consulted while she was being resuscitated with blood products in the ED, and she was promptly taken to the operating room for an exploratory laparotomy. This revealed approximately 2 liters of hemoperitoneum. She underwent a left salpingectomy for a ruptured ectopic pregnancy. She did well during her post-operative course and was discharged home on post-op day 3. She subsequently had a spontaneous vaginal delivery of a viable infant at 37 weeks.
A heterotopic pregnancy is characterized by the coexistence of an intrauterine and one or more extrauterine pregnancies.2 The incidence of a heterotopic pregnancy is about 1 in 30,000 natural pregnancies and increases to 1 in 100 in pregnancies resulting from assisted reproductive technologies (ART).3 The fallopian tube is the most common site of an ectopic pregnancy.2
It is important for emergency medicine, primary care, and urgent care physicians to consider the diagnosis of a heterotopic pregnancy in a patient with an IUP in the setting of hypotension, particularly in patients with a history of ART. While early diagnosis of an IUP usually rules out an ectopic pregnancy, a heterotopic pregnancy should still be on the differential as published reports of heterotopic pregnancies have noted that almost a third of cases had a previous, “falsely reassuring”, normal sonographic report of an IUP, as in our patient.4 Additionally, vital signs do no correlate well with the degree or shock or blood loss in all cases of ruptured ectopic pregnancies, and particularly (relative) bradycardia, as in our case even with significant hemoperitoneum, has been described for over 30 years in the literature.5–8
In conclusion, when performing a point of care obstetric ultrasound during the workup of a patient with suspected ruptured ectopic or heterotopic pregnancy, it is important to expand the exam to include FAST views to evaluate for hemoperitoneum and maintain a high index of suspicion so as not to miss early hemorrhagic shock even in patients with normal heart rate or bradycardia.