Introduction
A 24 year old Caucasian pregnant female presented to the doctor’s office for routine prenatal care at 35 weeks, 2 days gestation. Prior to this visit, there were no complications noted throughout the progression of this pregnancy. The patient complained of decreased fetal movement and ultrasound revealed absent fetal heart tones. A stillborn fetus was delivered the next day and Kleihauer-Betke test indicated severe fetal-maternal hemorrhage. This case is unique as it required a significantly larger dose of RhoGAM than the recommended empiric dose (12,000 IU’s in our case vs the recommended 1500 IU empiric dose). We performed an extensive literature review of fetal maternal hemorrhage, and we could not find a case report or study that showed previous use of such an amount of RhoGAM.
Description
The G2P1001 patient initially visited the OBGYN clinic for prenatal care at 6 weeks and 2 days of gestation where routine labs, ultrasound, cultures and pap smear were performed. She had four total ultrasounds over the course of this pregnancy and all were within normal parameters, including targeted ultrasound which was performed at 19 weeks and 5 days gestation. It showed no indication of hydrops fetalis or any other complications. The last ultrasound before the IUFD occurred was 7 weeks prior and found that the fetus’ weight was 66th percentile (1356 grams) with a heartrate of 135, normal amniotic fluid, and vertex presentation. The patient’s blood type is B negative and she has a history of anxiety/depression, splenectomy due to splenomegaly of unknown etiology, borderline tricuspid regurgitation, GERD, SVT, anemia and abnormal pap smear (ASCUS+HPV – colpo negative). Patient’s medications at the time included Toprol, Paxil, Temazepam and Protonix. Her first child was delivered vaginally at 38 weeks of gestation, 6 lbs 8 oz with no complications and a negative antibody screen during that pregnancy. Labs at approximately 28 weeks gestation revealed that the patient was negative for anti-D antibodies.
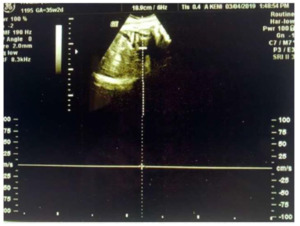
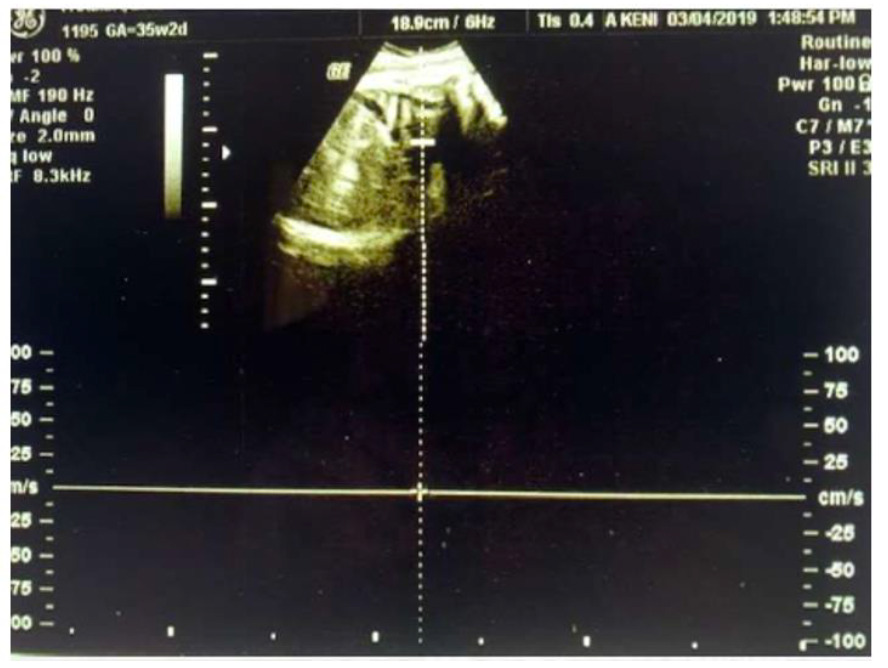
When absent fetal heart tones in this pregnancy were discovered, ultrasound also revealed edema around the fetus’s brain (Figure 2) and diaphragm (Figure 3), indicating hydrops fetalis. The fetus still showed to be in a vertex position with a normal amount of amniotic fluid upon further assessment. The patient was sent to labor and delivery where she was induced and given an epidural. She had a spontaneous vaginal delivery that produced a 5 lb 13 oz stillborn female at 35 weeks, 3 days. The placenta was sent to pathology for further assessment.
Pathology revealed the placenta weighed 645 grams, which is large for gestational age. A tri-vascular umbilical cord was noted with no evidence of funisitis. No significant infarcts were noted in the placenta.
A workup on the patient was performed to determine the cause of intrauterine fetal demise (IUFD). Her Kleihauer-Betke test was positive and estimated greater than 300 mL of fetal blood had mixed with maternal blood, leading to a diagnosis of fetal-maternal hemorrhage. KB test was confirmed via repeat test. That amount (300mL) of fetal blood loss indicates complete fetal exsanguination for a late pre-term infant. Further workup done after the stillborn was delivered revealed that the fetus’s blood was B positive, leading to a concern for possible isoimmunization in the patient. Initially, 11 vials (3,300 mcg or 16,500 IU’s) of RhoGAM was calculated for treatment of this patient. After consultation with a Maternal Fetal Medicine Specialist and historical literature review, a more conservative decision to use 8 vials (2,400mcg or 12,000 IU’s) of RhoGAM was made.
Type and screen of the patient’s blood was performed one month after the fetus was delivered and showed to be anti-D positive with a titer of 1, which is very low. Additional type and screen four times over the course of four years since the fetus was delivered proved to be anti-D negative. This means that the patient did not undergo isoimmunization, so her antibodies will have no bearing on future pregnancies that she may have.
Discussion
Normally, fetal blood and maternal blood are kept separate from each other during pregnancy. This is due to the layered blood barrier within the placenta that allows for gas and nutrient exchange to occur, but keeps blood cells from crossing due to their size. When this barrier fails to keep the blood separated, the fetus’s blood mixes with the patient’s. If the fetus loses a large amount of its blood supply (up to half or more), it can lead to intrauterine fetal demise (IUFD). Some causes of fetal-maternal hemorrhage include trauma, placental abruption, amniocentesis, or it may even be spontaneous.
In a case of fetal-maternal hemorrhage, if the patient is Rh negative and the fetus is Rh positive, then the patient’s body will begin creating antibodies. Typically, if the patient does not already have anti-D (Rh) antibodies built up, the development of these antibodies with the initial fetal-maternal hemorrhaging pregnancy will not create further issues with the fetus. If the patient gets pregnant again with a fetus that is Rh positive, her anti-D antibodies from the previous pregnancy will begin attacking the fetus’ red blood cells, causing a hemolytic condition known as Rhesus Disease. Rhesus disease can cause the fetus to become anemic, jaundiced, develop heart and brain damage, and even cause fetal demise.
Rhogam or Rho(D) immune globulin is made up of antibodies to the antigen Rho(D) present on some red blood cells. Rhogam works by blocking a patient’s immune system from recognizing the Rho(D) antigen. It is used to prevent isoimmunization in cases of fetal-maternal hemorrhage and it is ~99.8% effective per literature. It is often used in Rh negative patient’s and can be given both during and following a pregnancy.
Conclusion
Fetal-maternal hemorrhage should be considered in all cases of IUFD. It should also be considered in situations involving trauma. Additionally, signs of fetal hydrops should be screened for during any/all target, growth, or BPP ultrasounds during pregnancy. Incidental findings of hydrops would certainly warrant MFM evaluation and subsequent delivery of the fetus to prevent IUFD. To detect fetal-maternal hemorrhage, a rosette test is indicated to assess for the presence of D+ red blood cells in the patient if she is Rh negative. If the rosette test is positive, then a Kleihauer-Betke test should be performed to confirm and ultimately quantify how much fetal blood loss has occurred. The results of the KB test are used to calculate how much Rhogam is needed to be administered to the patient. Immediate delivery of the fetus should be performed once significant hemorrhage is confirmed to ensure the best possible chance for survival of the child.