INTRODUCTION
Squamous cell carcinoma (SCC) ranks second only to basal cell carcinoma as the most common cutaneous malignant skin condition across the globe. SCC typically presents as an erythematous scaly patch in its in situ form. Invasive subtypes often present as papulonodular but can display plaque-like, papillomatous, or exophytic characteristics. Most commonly, the root cause of SCC is attributed to actinic keratoses, resulting from excessive sun exposure.1 In recent years, however, immunosuppression has shown to be a major factor in tumorigenesis, with SCC emerging from areas of chronic inflammation.2
CASE REPORT
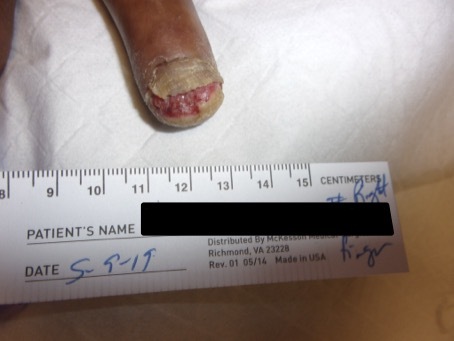
Patient is a 57-year-old male who presented to wound clinic after being referred by his primary care provider. Patient’s chief complaint was “finger won’t stay healed up” following a crush injury sustained while working on farm equipment. Upon the initial visit, the patient exhibited a 2.8cm (L) x 3.3cm (W) x 0.1cm (D) wound on his right second digit. Patient reported a 0/10 pain score despite having adipose tissue exposed with hypergranulation evident. The wound margins were well defined with only scant serosanguinous discharge. The wound was free of odor, eschar, or slough. Patient’s CBC and ESR were within normal limits. Clinical suspicion of osteomyelitis was confirmed on imaging. On the initial visit, the wound was cleaned thoroughly with normal saline, and a tissue culture was obtained. Silver gel dressing was applied, and Ciprofloxacin 750 mg BID was begun while awaiting final culture report. Subsequent culture reported Serratia marcescens and Escherichia coli, both of which were sensitive to Ciprofloxacin. The patient was then counseled on the importance of keeping the wound clean and dry, educated on the importance of smoking cessation, and scheduled to follow-up to wound clinic weekly. Figure 1 shows the wound at the initial clinic visit.
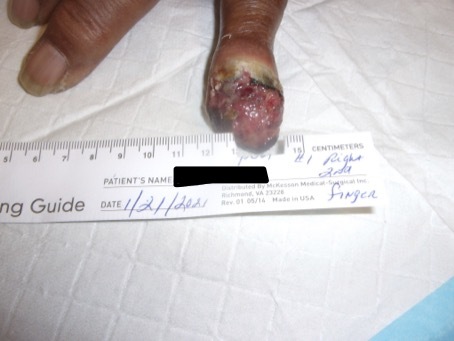
The patient initially responded well to sharp debridement, basic wound care practices, and the antibiotic regimen; however, at various intervals during maintenance and surveillance, the patient showed signs of cellulitis around wound margins. During each instance, the wound was re-cultured, and sensitivity reports continued to confirm that the correct antibiotic was being administered. The patient denied any new environmental exposures prior to these episodes. After inappropriate response despite treatment with appropriate antibiotics, the decision was made to obtain a biopsy. The biopsy result showed “poorly differentiated squamous cell carcinoma.” Upon the results of the biopsy, the patient was advised that the best course of action would be amputation of the distal phalanx. Figure 2 shows wound at final clinic prior to surgical intervention. The procedure was completed successfully with no complications. The patient was then referred to oncology, who agreed with negative margins and negative metastatic workup no further treatment was needed. At the time this report is being written, the patient has displayed no signs of recurrence.
DISCUSSION
A cutaneous malignancy arising from an ulcer, or otherwise damaged skin, is known as a Marjolin’s ulcer. These ulcers are most commonly associated with burns; however, the technical definition is “malignant degeneration arising within pre-existing scar tissue or even chronic inflammatory skin lesions.” These lesions are named for Dr. Jean Nicholas Marjolin, a French surgeon who noted the presence of villous atypia in burn scars. While these malignancies by and large turn out to be squamous cell carcinoma, they could be composed of other tumor types. Instances are rare with only 0.05% of all squamous cell carcinomas of the lower extremity being attributed to a Marjolin’s ulcer. Marjolin’s ulcers are 3 times more likely to develop in men than in women, and average age at diagnosis is in the 5th decade of life. The patient discussed falls into both of these parameters. While typically thought of in association with burns, Marjolin’s ulcers can also be associated with osteomyelitis. While rare, up to 1.7% of chronic osteomyelitis cases have been known to develop into cutaneous squamous cell carcinoma. At this time, the exact pathophysiology behind malignant transformation remains unclear; however, it is generally regarded that the causes are likely multifactorial. In patients with no metastasis, the prognosis is generally favorable with the overall 3 year survival rate between 65-75%. Mainstay treatment generally includes wide excision or amputation, depending on location.3 Informed consent was obtained from the patient.