Introduction
Myroides odoratum and odoratimimus are aerobic, non-fermenting, gram-negative bacilli.1 Growth can be observed on nutrient and MacConkey agars at room temperature (18 - 22°C) and normal body temperature (37°C).2 These organisms are widely distributed in natural ecosystems such as soil, fresh and marine waters, food, and sewage treatment plants.
The pathogenicity of Myroides spp. is unclear and is considered opportunistic. Most reported pathogenic cases are in immunocompromised hosts and declare broad antimicrobial resistance.3 Common regimens for treatment of COVID-19 include the use of corticosteroids and biologic agents like tocilizumab, both of which predispose patients to immunocompromise. Because of this, clinicians should consider the possibility of infection caused by unusual organisms, particularly when unresponsive to broad, empiric antibiotic therapies.
While infections with Myroides spp. are uncommon, infection types predominantly described to date are soft tissue and catheter-related infections.3,4 Far less common, yet more severe, infection types include pneumonia, ventriculitis, and endocarditis. Here we report a case of Myroides spp. bacteremia secondary to ventilator-associated pneumonia in a patient with COVID-19. This incidence of Myroides spp. pneumonia is only the fourth case to have been reported worldwide, the second case with concomitant bacteremia, and the first with meropenem resistance.3,5,6 Informed consent was obtained.
Case Presentation
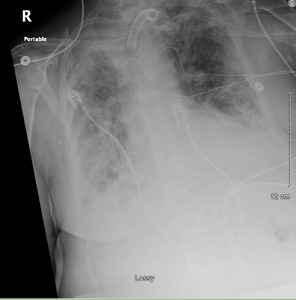
A 66-year-old female with no significant past medical history presented to the emergency department (ED) with a chief complaint of shortness of breath. She presented after approximately one week of symptoms with malaise, fatigue, and cough. On examination, she appeared anxious and in moderate distress with a respiratory rate of 39 breaths per minute (bpm) and pulse oxygen saturation (SpO2) of 81% on room air. She was placed on bilevel positive airway pressure (BiPAP). Laboratory tests were significant for a positive COVID-19 polymerase-chain-reaction (PCR) and elevated lactic acid (2.4 mg/dL) and inflammatory markers: ferritin (929.3 ng/mL), CRP (11.20 mcg/mL), and d-dimer (4.49 mcg/mL). Arterial blood gas (ABG) values following initiation of BIPAP were: pH 7.44, PaCO2 40 mmHg, PaO2 72 mmHg, O2 Saturation 95.1% on 100% FiO2. Chest Xray showed bilateral diffuse infiltrates consistent with acute respiratory distress syndrome.
She was admitted to the intensive care unit (ICU) with a working diagnosis of acute hypoxic respiratory failure secondary to COVID-19 pneumonia and likely superimposed bacterial infection. She was initiated on conventional therapies for COVID-19 at the time with dexamethasone 6 mg intravenously (IV) daily for 10 days and two doses of tocilizumab 8 mg/kg IV. Azithromycin and ceftriaxone were added empirically for suspected superimposed bacterial pneumonia. (Image 1) Blood and urine cultures were collected and eventually resulted in no microbial growth. Within 24 hours, the patient required intubation and mechanical ventilation for acute respiratory distress syndrome (ARDS).
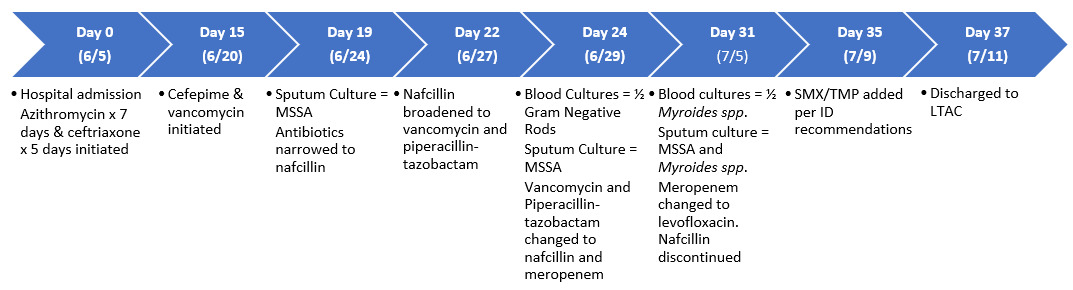
The patient showed mild, gradual improvement over the first two weeks; however, on day 15 of admission positive end-expiratory pressure (PEEP) requirements increased from 10 to 14 cm H2O, she became febrile (Tmax 37.8°C), developed mild leukocytosis (WBC 12 K/μL), and elevated D-dimer of 5.58 mcg/mL. Computerized tomography (CT) of the chest showed left lower lobe pulmonary embolism, moderate-sized right pleural effusion, and bilateral infiltrates. Chest tube was placed for parapneumonic effusion, therapeutic enoxaparin was initiated for pulmonary embolism, and empiric vancomycin and cefepime were started for suspected ventilator-associated pneumonia. The aforementioned interventions resulted in improved PEEP and FiO2. The antimicrobial regimen was de-escalated to nafcillin after sputum cultures showed methicillin-susceptible Staphylococcus aureus (MSSA) and Candida.
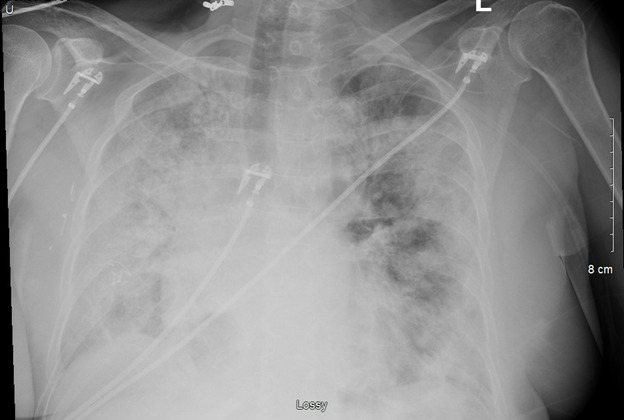
The patient’s condition began to decline again after 72 hours, as evidenced by elevations in WBC (peak 24.2 cells/μL), tempertaure (38.3°C), bandemia (10%), and persistent diffuse bilateral infiltrates on chest radiographs. (Image 2) Nafcillin was re-escalated to vancomycin and piperacillin-tazobactam, and pan cultures were performed. Sputum gram stain revealed gram-positive cocci (GPC), yeast, mold species, and gram-negative rods (GNR), and voriconazole was added. One of two blood cultures also showed GNR on gram stain. After no improvement in 48 hours, piperacillin-tazobactam was escalated to meropenem. The GPC again resulted MSSA, and vancomycin was de-escalated to nafcillin.
The GNR organism in sputum and 1 of 2 blood cultures finalized as Myroides spp. This was the first positive laboratory confirmation of this organism in our institution. It exhibited resistance to aztreonam, cefepime, ceftazidime, meropenem, and piperacillin-tazobactam. Susceptibilities included gentamicin, levofloxacin, and sulfamethoxazole/trimethoprim (SMX/TMP). (Table 1)
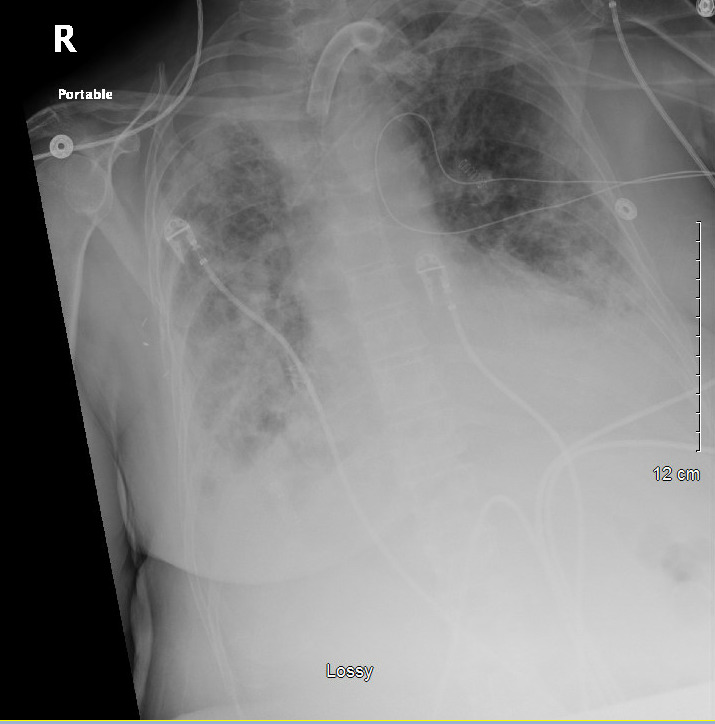
Meropenem was changed to levofloxacin 750 mg IV daily which resulted in resolution of fever and leukocytosis by day four. Infectious disease was consulted and added SMX/TMP 1 double strength (DS) tablet twice daily to levofloxacin to complete a 14-day course of antibiotics at discharge. (Figure 1) This recommendation was based on limited clinical experience in treating Myroides infections and prior case reports utilizing double antibiotic coverage. The patient was discharged to a long-term acute care facility on mechanical ventilation through tracheostomy tube with an FiO2 of 50%. (Image 3)
Discussion
Infections by Myroides spp. typically occur in immunocompromised patients, with cases of pneumonia being especially rare.3–7 Previous studies cite the association of these species with aquatic environments.5,8 The use of devices such as mechanical ventilators and urinary catheters create ideal environments for these organisms to thrive. Additionally, Myroides isolates demonstrate the ability to form biofilms in more clinically relevant temperatures (37°C).3,9 Together, the capability of biofilm formation and affinity for aquatic environments present a peculiar opportunity to develop an infection in patients receiving mechanical ventilation. Through the production of biosurfactant compounds, Myroides spp. gain the ability to invade deeper mucosa which facilitates the development of bacteremia.5
This genus has been historically reported as broadly resistant to beta-lactams, including carbapenems, with variable susceptibility to aminoglycosides, quinolones, and sulfamethoxazole.1 Resistance mechanisms are poorly understood, but include production of metalloenzymes and presence of efflux pumps. Speciation of the Myroides spp. isolated in our case was not performed; however, the pattern of resistance expressed is consistent with production of metalloenzymes. Prior reports of Myroides spp. pneumonia do not portray resistance to meropenem, which differs from our case.3,5,6 (Table 2) Our patient was subjected to a transient state of immunosuppression secondary to treatments with dexamethasone and tocilizumab for COVID-19, which likely facilitated onset of bacterial pneumonia and bacteremia. Throughout the treatment course, the patient was treated to no avail with preferred first-line agents for pneumonia. Susceptibility testing ultimately demonstrated resistance to our first-line agents.
In the climate of COVID-19 infections with a sizable number of patients requiring mechanical ventilation, the possibility of infection by this rare, opportunistic, pathogen should not be discounted in pneumonia unresponsive to commonly used broad-spectrum antibiotics. Consideration for resistant pathogens should be heightened given the common use of immunosuppressing agents in the treatment of COVID-19.
CRediT Statement
Ashley Hawthorne: Conceptualization, Investigation, Data curation, Writing – Review & Editing, Visualization, Supervision, Project administration; Brittany Walley: Investigation, Resources, Data curation, Writing – Original Draft, Visualization; Dipti Baral: Conceptualization, Investigation, Writing – Review & Editing, Visualization.
Acknowledgements
None.