A 56-year-old Caucasian male with a past medical history of laparoscopic cholecystectomy in 2012 was seen and evaluated in outpatient clinic for new onset painless jaundice for three days. Prior to this, the patient had one month complaint of abdominal pain that was associated with pale stool, nausea, and vomiting. He had gone to an emergency department (ED) for these symptoms. Part of the workup included an abdominopelvis CT scan which was negative for intra-abdominal pathology. He was discharged with oral antinausea medication and asked to follow up with his primary care physician (PCP).
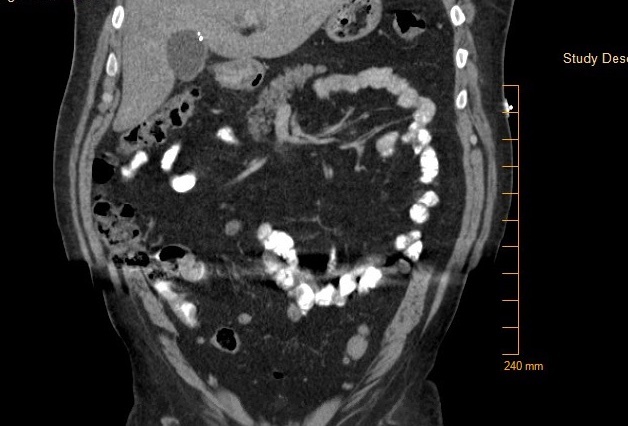
At his next visit with his PCP, however, he complained of pruritus, loss of appetite, 30 lb weight loss, weakness, increased yellowing of eyes, and worsening abdominal pain for 3 – 4 days. He was sent emergently to the ED, and a repeat CT scan of the abdomen/pelvis showed diffuse fatty infiltration of liver, mildly distended gallbladder with intra and extra hepatic biliary ductal dilatation and a common bile duct measuring up to 2 cm. No definitive filling defect was seen within the gallbladder. Ultrasound of the abdomen demonstrated dilated intrahepatic and extrahepatic ductal dilatation and uncomplicated small gallstones within the gallbladder but without choledocholithiasis or a discrete mass identified.
The patient stated that he had not smoked cigarettes. He denied use of alcohol and stated that he was a retired military veteran with negative family history of malignancies. He stated that he had a cholecystectomy nine years ago, while on the Air force military base and denied any post-operative complications.
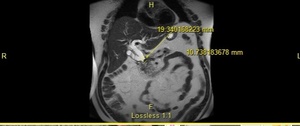
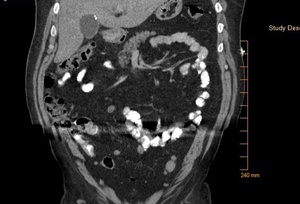
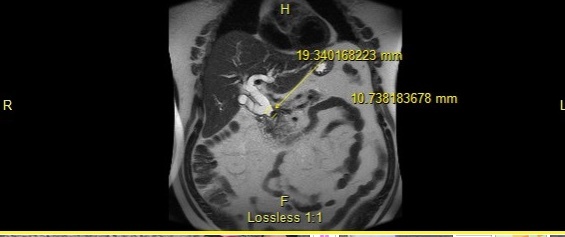
His laboratory values were significant for elevated total and direct bilirubin (22.4 and 15.9 mg/dl). Additional lab values include – an AST (137 U/L) and ALT (232 U/L), and an abnormally elevated Lipid panel with LDL (263 mg/dl), triglyceride (357 mg/dl), and total cholesterol (346 mg/dl). On day three of admission, the patient underwent an endoscopic retrograde cholangiopancreatography (ERCP) with findings significant for multiple gallstones in the common bile duct (Fig. 1 - 4) consistent with Mirizzi syndrome.
On the ERCP, patient had outpouching in the cystic duct. A stent was placed in the common bile duct (CBD). The patient’s direct bilirubin decreased from 7.4 mg/dl to 5.9 mg/dl. The patient was scheduled to follow up with gastroenterologist in two to three weeks for the removal of the CBD stent, and he improved markedly post-stent placement. He was asymptomatic on discharge.
Discussion
Mirizzi syndrome is obstruction of the common hepatic duct from a stone impacted on the gallbladder infundibulum or cystic duct remnant. It has been classified into five variants (Table 1) based on the Csendes 2007 classification.1 It usually presents with right upper quadrant pain, with or without jaundice and fever.2 The most commonly used studies for diagnosing Mirizzi syndrome are the ultrasound, computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP) but the endoscopic retrograde cholangiopancreatography (ERCP) is the most sensitive.3 It is reported to have a 100% sensitivity,3 and as seen in this case can be diagnostic for Mirizzi syndrome.
There is no standard approved treatment for Mirizzi syndrome. There are varied opinions on the best ways to manage the disease in the literature. Laparotomy is noted for better visualization of the anatomical structure and hence less biliary tract injury.4 A laparoscopic approach preferred especially with good surgical skill and associated with advantages of shorter recovery time and in-hospital stay,5 and a downside of high risk of conversion from laparoscopy to laparotomy.6 A combined endoscopic and robotic approach is sometimes indicated. Finally, patient specific management depends on the type of Mirizzi syndrome.
This patient had an atypical presentation of post laparoscopic cholecystectomy pain and had an ERCP that showed outpouching of the cystic duct and thus can be classified as post cholecystectomy Mirizzi syndrome (PCMS). PCMS occurs when a stone in the remnant cystic duct lying parallel to the hepatic duct impinges on the hepatic duct. Its presentation resembles biliary pathologies and requires a high index of suspicion. It can also be diagnosed by confirmatory imaging studies or intra operatively. It can also occur in rare cases when surgical polymeric clips move up the cystic duct or cystic artery.7
This patient presented nine years after laparoscopic cholecystectomy which is consistent with the range of a few days to 40 years reported by other authors.8 He had weight loss, pruritus, and abdominal pain which are found only in a minority of patients, as shown by a systematic review of 64 cases of PCMS.8 In addition, he had nausea, vomiting, and jaundice which are found in majority of Mirizzi syndrome cases reported in the literature.8
The diagnosis of Mirizzi syndrome requires a high index of suspicion, and a multi-disciplinary approach incorporating gastroenterology, primary care, and radiology. The access to high quality ERCP may be a limiting factor in sub-urban and rural hospitals, but their use is required for a rapid and reliable diagnosis of Mirizzi syndrome, and possible therapeutic intervention as demonstrated in the index case.
Informed Consent
Informed consent was obtained from the patient to publish this case report.