Introduction
Progressive multifocal leukoencephalopathy (PML) is a rare but severe demyelinating disease caused by John Cunningham (JC) virus in immunocompromised individuals. With the advent of effective antiretroviral treatment (ART) and resulting preservation of immune function, PML has become a rare clinical diagnosis among patients living with human immunodeficiency virus (HIV). After ART became widely available, the incidence of PML declined from 14.8 per 1,000 person-years in 1996 to 0.8 per 1,000 person-years in a European cohort.1 Due to a lack of antiviral therapy against JC virus, initiation or maintenance of ART is the only known therapeutic approach. Even with ART, the 1-year mortality rate is approximately 50%.2
Patient Information
A 59 year-old-female with a history of HIV and hypertension presented with vision loss and forgetfulness of two months’ duration, which progressed to bilateral blindness accompanied by memory loss and cognitive decline. Diagnosed with HIV in the mid-2000s in her 40’s, the patient discontinued all HIV care after a brief period of engagement. She resumed ART with bictegravir, emtricitabine, and tenofovir alafenamide (commonly co-formulated as Biktarvy) on presentation, with a cluster of differentiation 4 (CD4) count of 87 cells/µL and a viral load of 2960 copies/mL. Her medical history revealed no prior diagnosis of PML.
The patient lived with a supportive family, did not use tobacco, and consumed alcohol occasionally. Prior to her decline, the patient had been independent, working as a supervisor, and performing all activities of daily living. Her worsening condition led to job loss and a decline in her quality of life, with her daughter noting episodes of disorientation and forgetfulness.
Informal verbal consent for the publication of this case report and associated clinical details was obtained from the patient’s family member.
Clinical Findings
By March 2023, the patient’s cognitive decline and memory impairment significantly worsened. Despite outpatient follow-up with ophthalmology, her vision continued to deteriorate. Given the progression of her symptoms, the patient was advised to present to the hospital.
On admission, the patient exhibited significant neurological deficits, including disorientation, difficulty finding words, and frustration during interactions. Physical examination revealed no acute distress, with stable respiratory and cardiovascular findings. Neurological examination displayed signs of progressive cognitive impairment.
Timeline
A detailed timeline of key clinical events is presented in Table 1.
Diagnostic Assessment
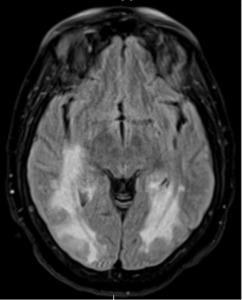
The diagnosis of PML was based on magnetic resonance imaging (MRI) findings and clinical presentation, including progressive vision loss and neurological decline. Prior to her hospitalization, an outpatient brain MRI revealed extensive T2/FLAIR hyperintensities in the parieto-occipital white matter and splenium of the corpus callosum, concerning for PML (Image 1).
A repeat inpatient brain MRI consistently indicated PML, displaying mild progression of the extensive abnormal signal without significant mass effect or enhancement. A lumbar puncture revealed cerebrospinal fluid with 3,100,000 copies/mL of JC virus, confirming the diagnosis.
While MRI findings were also consistent with Posterior Reversible Encephalopathy Syndrome (PRES), this was less likely. Immune Reconstitution Inflammatory Syndrome (IRIS) was ruled out due to the lack of imaging enhancements typical of IRIS and the onset of symptoms prior to ART reinitiation.
Therapeutic Interventions
The patient was restarted on ART with bictegravir, emtricitabine, and tenofovir alafenamide (Biktarvy) on initial presentation to address her uncontrolled HIV. As her neurological condition worsened, supportive care was prioritized. Three months after initial presentation, she experienced left-side hemiplegia and expressive aphasia. Her family opted for palliative care with a focus on comfort.
Follow-Up and Outcomes
Despite ART reinitiation, the patient’s condition deteriorated rapidly. Her progression of bilateral blindness, expressive aphasia, and hemiplegia profoundly impacted her quality of life. Given her poor prognosis, her family initiated hospice care, with a care plan focused on comfort measures. She ultimately passed away while under hospice care.
Discussion
This case highlights the devastating consequences of delayed ART in patients living with HIV. PML, while rare, remains a life-threatening opportunistic infection associated with severe immunosuppression. In the era of effective ART, such outcomes are largely preventable with early engagement in care and sustained treatment adherence.
Although PML has become less common, it still occurs in patients with advanced immunosuppression or poor adherence to therapy. An observational study in India found that, while PML remains associated with severe morbidity, mortality declined significantly with early diagnosis and timely initiation of ART.3 In the southern United States, including Mississippi, persistent disparities in access to HIV care continue to contribute to delayed treatment initiation, suboptimal adherence, and poor clinical outcomes.4 These patterns reflect an ongoing public health challenge in underserved and resource-limited settings.
The progression to PML in this patient underscores the tragedy of preventable outcomes in the modern era of effective HIV management. Her clinical course illustrates how, despite the availability of effective ART, delayed re-engagement in care can lead to devastating neurological decline. Prior to symptom onset, the patient was employed, independent in daily activities, and living with family support—emphasizing how quickly PML can disrupt functional status and quality of life.
While current HIV therapies are highly effective, late-stage complications like PML serve as a stark reminder of the importance of early diagnosis, consistent treatment adherence, and robust follow-up systems for individuals living with HIV. In the modern era of effective HIV therapies, no patient should die from preventable complications like PML.
Disclosure
Thomas Dobbs serves on the editorial board of the JMSMA but was not involved in any of the decisions regarding review of the manuscript or its acceptance.