Introduction
Paraquat is a bipyridyl herbicide that is popular in U.S. agriculture due to its broad-spectrum herbicidal effects. Although human ingestion is rare, it is extremely toxic, and mortality rate is high.1 Paraquat exerts its toxic effects mainly through the production of reactive oxygen species (ROS) and subsequent cellular damage, particularly significant in the lungs.2 With no known antidote, time to treatment, especially the initiation of hemodialysis or hemoperfusion is an important prognostic factor.3 Therefore, clinicians in regions with high prevalence of agriculture and paraquat use should consider paraquat poisoning in patients presenting with renal and pulmonary symptoms following the ingestion of an unknown chemical and should be familiar with standard treatment protocols. Protocol should include contacting the poison control center if poisoning is suspected.
Case Report
A 58 year old Causasian male presented to the local emergency department (ED) with abdominal pain, nausea, and vomiting 8 hours after intentionally ingesting approximately 30 milliliters (mL) of paraquat (Gramoxone) in a suicide attempt. The patient was administered activated charcoal in the ED and poison control was contacted. The recommendations included supportive care only, given the elapsed time since ingestion and the absence of a specific antidote.
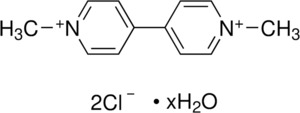
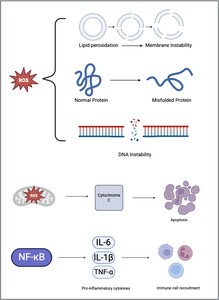
Upon initial evaluation, the patient complained only of nausea. A chest X-ray [image 1] and initial laboratory data [fig 1] were within normal limits. The patient was admitted to the ICU for continued supportive care and further monitoring. He was initiated on high doses of vitamin C, vitamin E, and N-acetylcysteine.
By day 2, the patient’s vital signs, including O2 saturation [fig 2], remained stable. He began to complain of a mild sore throat and had developed acute kidney injury [fig 1]. The patient was assessed by nephrology who did not recommend dialysis due to length of time since ingestion.
On Day 3, renal function continued to decline and acute elevation of liver enzymes was noted. [fig 1]. The patient continued to complain of worsening throat and mouth pain and was started on a mixture of aluminum/magnesium hydroxide, diphenhydramine and viscous lidocaine (magic mouthwash) and morphine for pain control.
On day 4, respiratory status remained stable but throat/mouth pain worsened and the patient developed an erythematous oropharynx with white patches of sloughing epithelium, a phenomenon coined “paraquat tongue”. Labs revealed a continued decline in renal function and a persistent elevation in total bilirubin, despite improvement in liver transaminases. [fig 1]
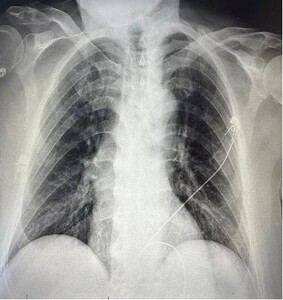
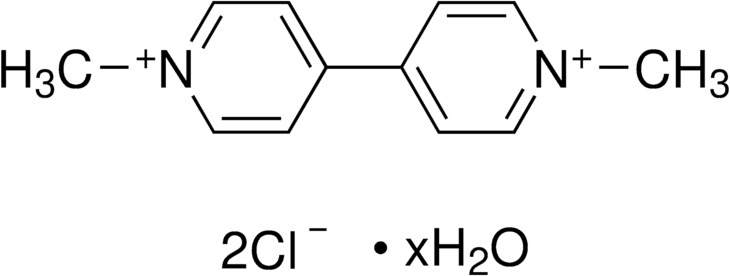
By day 5 post-ingestion, the patient continued to complain of worsening throat/mouth pain and was getting little relief with the mixture of aluminum/magnesium hydroxide, diphenhydramine and viscous lidocaine mouthwash or opioid pain medications. Renal function continued to decline and hypoxemia developed, with O2 saturation dropping to 85% on room air [fig 2], relieved with O2 via nasal cannula. Chest X-ray revealed bilateral peripheral infiltrates on day 5. [image 2]
By day 6, hypoxemia worsened with oxygen saturations in the 70s[fig 2] despite high flow oxygen. The patient became obtunded, and the family requested DNR status and hospice care. Unfortunately, the patient expired the following morning, 7 days after ingestion.
Discussion
Paraquat is mainly used for grass control and crop desiccation prior to harvest.4 All paraquat-containing compounds are listed as Restricted Use Pesticides in the United States that can only be used by licensed individuals.1 Paraquat poisoning is a significant public health problem worldwide, especially in developing countries. There is a much lower incidence of exposure in the United States, but several poisonings still occur annually.4 Most cases of paraquat poisoning are from intentional consumption during a suicide attempt. Accidental ingestions may occur when paraquat is placed in unlabeled or mislabeled beverage bottles.5 Paraquat is highly toxic with no known antidote.
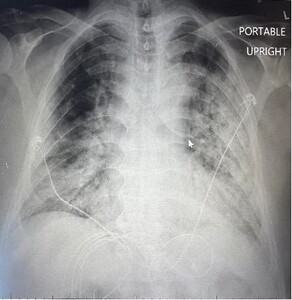
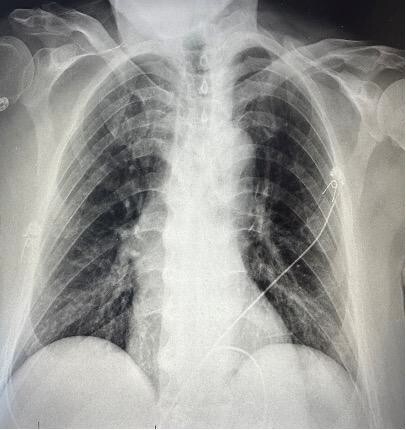
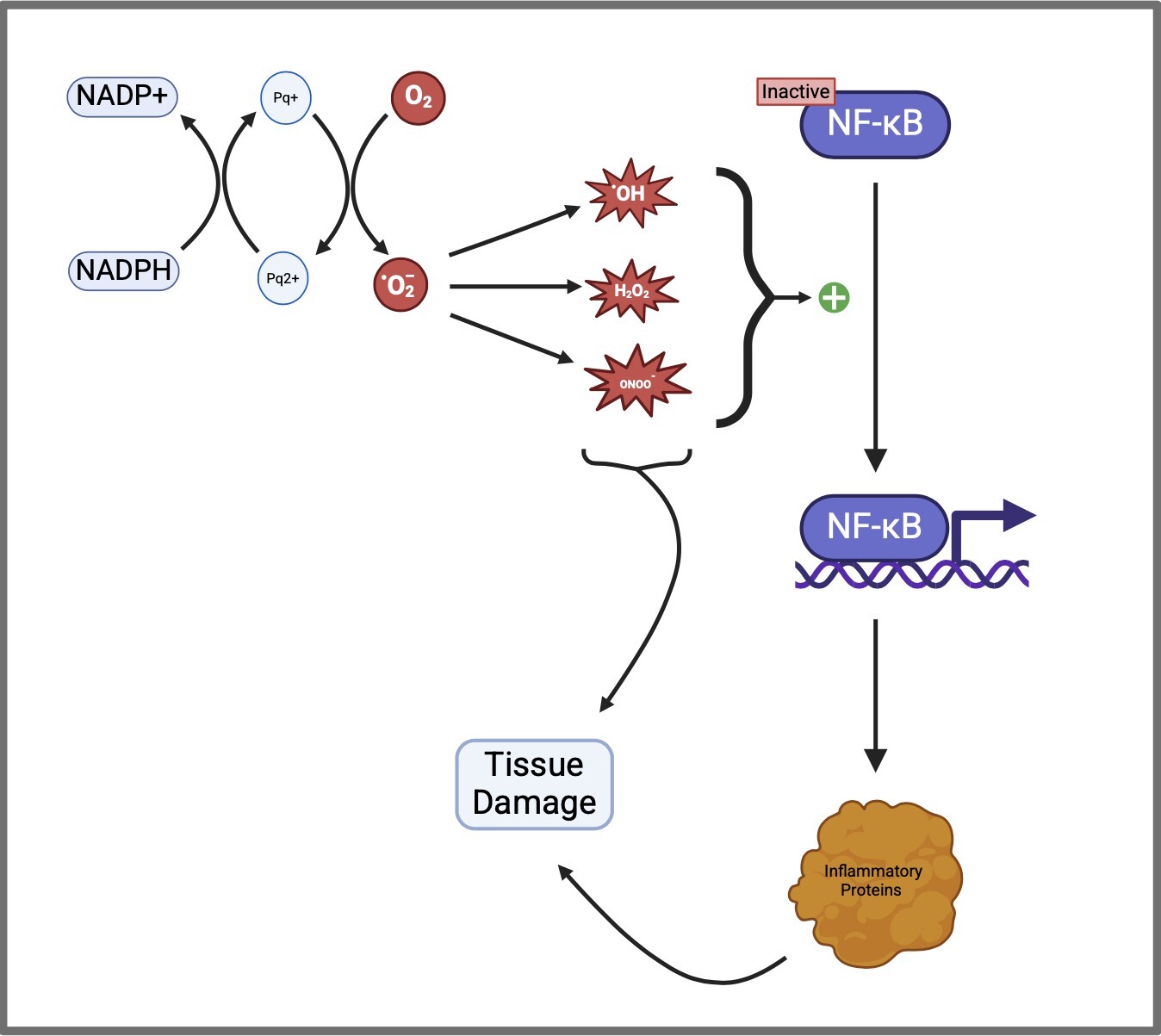
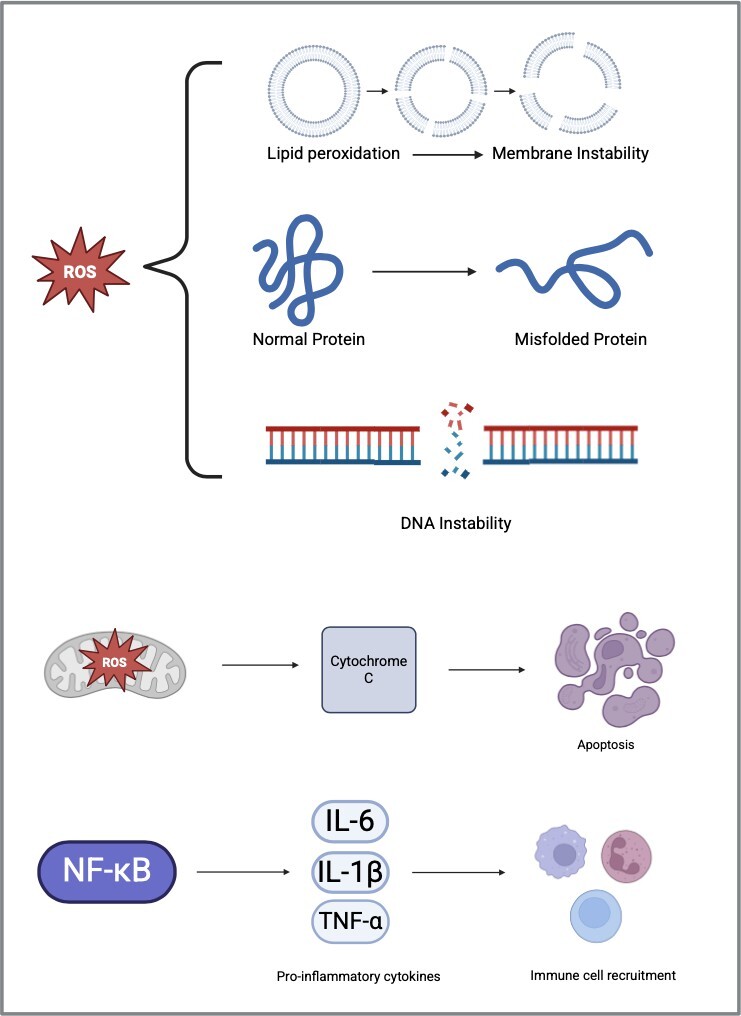
After ingestion, it is rapidly distributed to the lung, liver, and kidneys, with lungs and kidneys being the primary target organs. It is excreted in both bile and urine.4 Less than 20% of the ingested dose is absorbed in the stomach. Paraquat is caustic, and ingestions cause direct injury to the gastrointestinal tract resulting in ulcerations and epithelial sloughing (i.e., paraquat tongue).3 Paraquat’s toxicity results from its ability to undergo reduction-oxidation (redox) cycling to generate reactive oxygen species (ROS) [fig 3]. Once inside cells (ex. hepatocytes, pneumocytes) paraquat is reduced by nicotinamide adenine dinucleotide phosphate (NADPH) to form paraquat radicals (Pq+) which subsequently reduces O2 to form superoxide (O -).
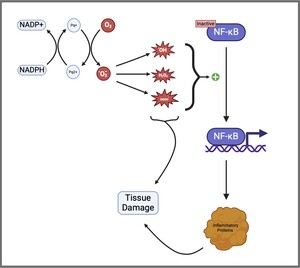
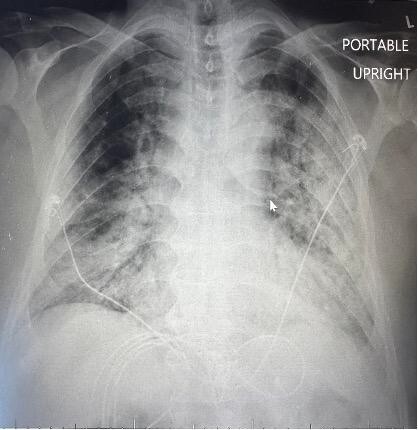
Superoxide can then give rise to several ROS such as hydroxyl free radical (OH-), hydrogen peroxide (H2O2), and peroxynitrite (ONOO-). These ROS cause widespread damage to lipids, proteins, and DNA leading to cellular dysfunction and death. In addition to their direct effect on cellular function, the ROS generated from paraquat activates nuclear factor kappa B (NF-KB), a gene promoter highly involved in pro-inflammatory responses. This process ultimately results in tissue damage through various mechanisms such as mitochondrial toxicity, oxidation of NADPH, apoptosis, and activation of numerous cytokines [fig 4]. These mechanisms promote inflammatory changes and vitiate antioxidant defenses.
Within hours of ingestion, renal clearance rapidly declines. Pulmonary toxicity typically occurs 2-6 days after ingestion. Paraquat slowly accumulates in the lungs due to the abundance of organic cation transporters in type II alveolar cells. The oxidative damage initially results in acute alveolitis, but rapidly progresses to pulmonary fibrosis.2
Our patient presented with a classic case of paraquat poisoning. Acute kidney injury developed 2 days post-ingestion, with pulmonary involvement becoming evident by day 3, contributing significantly to his clinical deterioration. By day 4, oropharyngeal lesions became apparent, along with continued decline of both renal and pulmonary function. The patient succumbed to toxicity on day 7 due to acute hypoxemic respiratory failure, a finding prominent in paraquat-related deaths.
Due to the severe toxicity of paraquat, limited treatment options are available and more than often futile. Initially, emphasis should be placed on the principles of basic life support (airway, breathing, circulation). Activated charcoal is a common treatment for numerous poisonings.
Activated charcoal works by absorbing the noxious substance onto its surface and thus preventing absorption through the gastrointestinal tract.6 As mentioned earlier, less than 20% of paraquat is absorbed in the stomach, so activated charcoal may be of little benefit, even if given early. Hemodialysis may be helpful if started within 2 hours post ingestion and there is no pulmonary involvement.2 Antioxidants (Vitamin E, Vitamin C, N- acetylcysteine) are used for their free radical scavenging properties. Immunosuppressive drugs (Dexamethasone, cyclophosphamide) have been used in an attempt to counteract the massive inflammatory response. Despite the utilization of numerous treatment modalities, including early hemodialysis, mortality from paraquat remains high after ingestion. Ingestion of amounts greater than 30 mL of 20% paraquat solution is generally fatal.2