Introduction
Breast Cancer and Radiation Therapy
Of all malignant cancers, breast cancer is the most common type treated with radiation therapy (RT) in the United States. The American Society for Radiation Oncology (ASTRO) published guidelines in 2018 to encourage evidence-based practices for radiation of breast cancer patients.1 These guidelines highlight the advent of hypofractionation resulting in complete radiation courses within 3 weeks as opposed to conventional 5 weeks. Within these guidelines, key questions were addressed regarding preferred fractionation for the treatment of whole breasts and tumor beds. Hypofractionation (typically either 40 Gy in 15 fractions or 42.5 Gy in 16 fractions) is preferred for whole breast irradiation (WBI). Additional criteria provide conditional recommendations for conventionally fractionated boost doses (10 Gy in 4-5 fractions) or partial breast irradiation (PBI). Specific dosimetric approaches and planning guidance were also outlined, including recommendations for heart sparing techniques. However, many practitioners remain either unaware of or hesitant about the value of new regimens regarding treatment outcomes when compared with more familiar conventional courses.
This work describes collaboration among radiation oncology centers in Mississippi to evaluate the implementation of evidence-based practice recommendations within Mississippi and to identify barriers to adoption of evidence-based guidelines as a first step towards improving practice in the state. European data published by Ratosa et al. described variability in adoption of moderate hypofractionation (MH) for breast radiation among surveyed centers.2 Survey results published in 2022 indicate that, across the United States, the use of hypofractionation and other recommended breast radiation practices has increased significantly but does not yet represent the majority of practice.3 This study evaluates local practice among radiation oncology centers throughout Mississippi by identifying RT patterns of practice as well as barriers to adoption of moderate hypofractionation for breast cancer treatment. The intention is to ascertain whether practice patterns in Mississippi compare favorably or not with those international and domestic. By virtue of data collection among peers, this work also lays foundation for further collaboration among local clinicians for promoting current and appropriate cancer care for patients in Mississippi.
Mississippi Radiation Center and Breast Cancer Statistics
As of 2020, Mississippi supported 24 radiation therapy centers which utilized (as of 2022) a total of 36 radiation oncologists.4 Breast cancer is prevalent in Mississippi. Of the 15,145 new cases of invasive cancer diagnosed in 2020, 2,141 were female breast cancer patients, or 14.1% of the total number of new cases. This compares to 1,660,481 new cases and 247,960 (14.93% of total) female breast cancer patients, both nationally in 2020. In 2020, 3,062 Mississippians died from cancer, including 501 breast cancer patients.5 For the same time frame, 602,350 Americans in general died from cancer, and 42,275 (or 7.02%) of those were from female breast cancer. Economic diversity and disparity, as well as rural geography, provide unique challenges to aligning feasible radiation therapy approaches to best practice recommendations in Mississippi patients and communities.6,7 This body of work not only highlights varied practice approaches for breast cancer radiation treatments within our state, but it also serves as catalyst to bridge the gap among radiation centers statewide by promoting collaboration among clinicians to improve quality of radiation care for all disease sites.6
Methods
With IRB approval (IRB UMMC-IRB-2022-129), an anonymous, 40-question electronic survey was distributed to radiation oncologist physicians practicing in the state of Mississippi. Twenty-two questions were multiple choice with the remaining being “check all that apply” with the addition of a free-form text in the event that “other” was chosen. Physicians were personally contacted via telephone before survey distribution to state the purpose of the survey and to initiate personal connection with the practitioner. Out of the 36 total physicians contacted, some (3) declined participation upfront, due to either lack of breast cancer patients or limited desire to fill out a survey. Participation in the survey was considered informed consent per the IRB-approved survey method and survey request communication. IBM SPSS Statistics software version 29 (statistical package for the Social Sciences Statistical Software; SPSS Inc. IBM Corporation, Armonk, NY) was used for data analysis and visualization.8 Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Mississippi Medical Center.9,10 REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources. The entire survey is attached as an appendix item. The survey results have been reported following the CROSS formalism.11
While the primary ASTRO recommendations address the need for preferential use of the hypofractionation regimen in whole breast, boost prescriptions, and contouring of targets and normal tissues, additional questions of interest were included in the survey; they were, however, not used to evaluate a compliant practice. Nonetheless, these additional items are expected to be meaningful to radiation oncology practitioners. In general, the goal was to determine the pattern of practice among the survey respondents.
Results
General Demographics
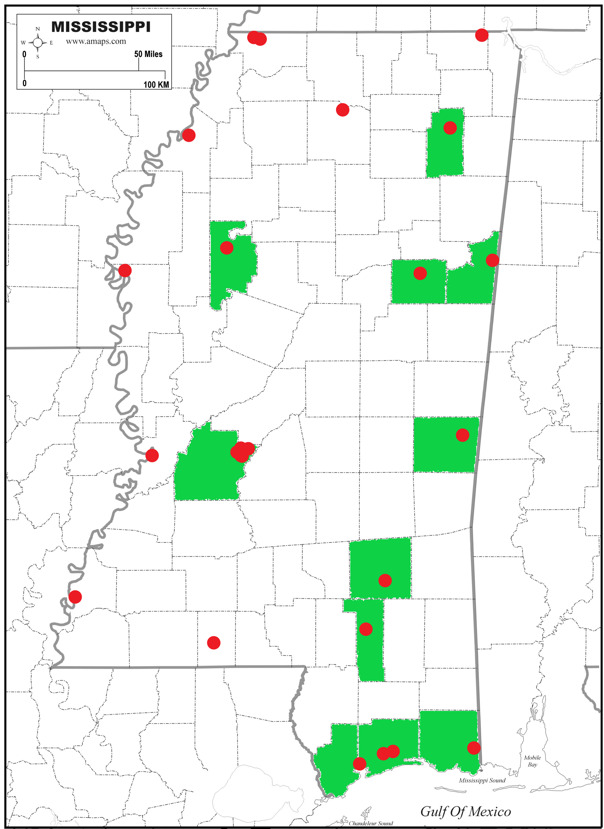
A summary of key results can be seen in Table 1. Also, areas recommended by guidelines are indicated in Table 1 versus the survey results. One of the 18 surveys was incomplete, so portions of presented data only represent 17 survey responses. Figure 1 indicates geographic distribution of the RT centers (red) and the counties with responding physicians (green). Of responding physicians, 12 were hospital-based physicians, 3 worked in free-standing cancer centers, 2 were employed in academic cancer centers, and 1 was associated with a military hospital. Lowndes, Leflore, Lee, Oktibbeha, Lauderdale, Jones, Jackson, Harrison, Hancock, Forest, and Hinds counties were represented. Participants who did not respond included those from the Jackson VA hospital and other community practices. Interestingly, many of the non-participating institutions exist on the periphery of the state. Due to the low number of responses even though response rate was high, only descriptive statistics were run and reported.
General Practice
See Table 1 for the case rates per month per institution per month. Most physicians shared breast cancer census among their practice partners with only four indicating that they are the sole physician responsible for breast patients at their institution. Fifteen physicians utilized multidisciplinary tumor boards for all or at least non-standard breast patients, while two physicians did not utilize tumor board. One physician indicated that RT decisions were guided by departmental new patient/chart rounds. Regarding peer review, 7 physicians indicated all radiation plans undergo peer review; two physicians utilize peer review more than half of radiation treatment plans. Further, 6 physicians use peer review less than half the time, and 2 physicians never utilize peer review for radiation treatment planning of breast cancer.
Hypofractionation
Per Table 1, it can be seen that a majority (61.1%) prefer hypofractionation when appropriate. One physician specifically stated a preferred unfamiliar regimen of 45 Gy in 20 fractions. Twelve (66.7%) physicians reported use of moderate hypofractionation for more than half of treated breast patients, with 3 exclusively using moderate hypofractionation. Six physicians used moderate hypofractionation less than half of the time, with 2 physicians never using hypofractionation. Eight physicians reported occasional use of ultra hypofractionation over 1 week, with 10 physicians never using this regimen. All physicians preferred conventional fractionation for postmastectomy patients, with 4 physicians using moderate hypofractionation in the postmastectomy setting occasionally.
Breast RT Strategy
Internal mammary lymph node coverage was variable. Eight physicians stated internal mammary nodes were covered less than 25% of the time when performing regional nodal radiation. Two physicians stated they included internal mammary nodes greater than 75% of the time when performing regional nodal radiation. Eight physicians stated internal mammary nodes were covered approximately 50% of the time when performing regional nodal radiation.
Thirteen respondents stated partial breast irradiation (PBI) was offered to appropriate patients. Four respondents did not offer partial breast irradiation, with 3 of the 4 stating this was due to unavailability of technique. Nine surveys reported PBI was completed with IMRT/VMAT. Seven surveys reported PBI was completed with targeted brachytherapy. Six surveys reported PBI was completed using 3D conformal radiation techniques. Seven responders used ASTRO guidelines for PBI criteria. Seven responders used NCCN guidelines for PBI criteria. Six responders reported ABS was used for PBI criteria.
Various heart sparing techniques are utilized across Mississippi institutions which conforms to guidelines. Deep inspiratory breath hold was not used or available in many survey responses due to lack of trained staff, lack of equipment, increased treatment time, and financial reasons. The prone setup technique was used by 1 physician indicating > 75% usage.
Consideration of omission of breast RT after breast conservation was indicated based on several factors: age (14 responders), T1 without risk factors (10 responders), comorbidities (8 responders), or DCIS with no risk factors (7 responders) Three physicians said they never or rarely recommend omission of breast RT after breast conserving surgery.
Contouring and Plan Review
Regarding organ at risk (OAR) delineation, all 17 responding physicians indicated they contour the whole heart, while 16 contour the ipsilateral lung. More than half contour the whole lung, spinal cord, contralateral lung, and contralateral breast. Only 2 physicians, however, contour cardiac substructures such as the left anterior descending artery and the left ventricle. Three physicians specified they contour OARs less than 25% of the time; all other physicians indicated contouring of OARs were completed for more than 75% of patients (1) or for all patients (14). During plan evaluation, most physicians review mean heart dose (13) with a handful also reviewing various volumetric dose features. Only 2 physicians indicated reviewing cardiac sub-structures. For the ipsilateral lung dosimetry review, most evaluate the volume of lung receiving 20 Gray (15); mean lung dose was the preferred dosimetric evaluation by 7 reviewers.
Almost all physicians reported delineating the lumpectomy bed (16) and whole breast (14), and most also delineated the whole chest wall (9), lymph node levels and regions (10), and the supraclavicular nodes (10). Three physicians reviewed breast RT plans qualitatively looking for 90-95% isodose line to cover the whole breast, while the rest (14) reviewed dose volume histogram metrics of their target volumes at various levels. Three MDs generally accept a 110% hotspot (of prescription dose) while 8 prefer 107% hot spot and 6 require less than 105% hotspot. Guidelines recommend minimizing the volume of breast receiving 105% of the prescription.
Discussion
Hypofractionation Utilization
Utilization and preference of hypofractionation is mixed within our survey results from Mississippi physicians. While hypofractionation may be somewhat underutilized, a majority of surveyed Mississippi radiation oncologists (>60%) prefer the technique for whole breast radiation. Common barriers to hypofractionation include toxicity concerns and financial concerns regarding reimbursement. Hypofractionation can be a cost-effective solution when used appropriately.12,13 One study projected a savings of $13.6 million dollars if 10,482 patients had been treated with hypofractionation when eligible.12 Mississippi, as a poor state with median income of only $49,111 and 19.4% of households living in poverty,14 could be an ideal target for the implementation of evidence-based, cost-effective medical care. Many survey responders are utilizing hypofractionation even outside the academic setting, suggesting that private practice utilization of hypofractionation is feasible. Regarding fear of toxicity using higher daily doses of radiation, it is possible that the publication of this data of practice patterns among peers may influence other Mississippi practitioners in adopting hypofractionated treatment techniques. These results may be relatively generalizable within Mississippi due to the high response rate; however, the generalizability may be limited based on the bias of physicians represented in the survey and those who were not.
Breast RT Complexity
Breast radiation therapy has evolved from the 2-dimensional treatment era, now with incorporation of wedges with traditional tangents, field in field planning, and IMRT. Volumetric delineation of target volumes and organs at risk with dose volume histograms have improved dose coverage to target structures while sparing normal tissues. The availability of published protocols and guidelines have served to educate regarding constraints for various organs at risk to improve long-term outcomes. Late toxicities from radiation therapy can be significant, and improvement in radiation techniques may reduce long-term complications in breast cancer survivors.15–17 It is reassuring to see that the majority of survey responses indicate utilization of modern techniques and dosimetric evaluation for breast cancer treatment in Mississippi.
Conclusions
Overall, it appears that most Mississippi radiation oncology physicians are following recommended practice guidelines regarding breast cancer radiation treatments. This conclusion should be verified with future surveys with improved response rates among Mississippi physicians. Current survey responders appear to be seeking optimal care for their breast cancer patients, taking measures to reduce toxicity to normal organs at risk with treatment fractionation and setup. Strategies to improve breast cancer radiation treatments within the state could include improving availability to treatment techniques, such as DIBH, as well as promotion of collaboration amongst radiation oncology physicians to allow for shared experience to successfully improve cancer care throughout Mississippi.