1. Bone lesions identified on radiographs encompass a variety of benign and malignant entities.
Radiographs can reveal numerous types of bone lesions, each with wide-ranging clinical implications.1 It is useful to classify lesions as aggressive or non-aggressive. Aggressive lesions include fast-moving, destructive processes like malignancy and infection, which must receive appropriate treatment. Non-aggressive lesions are typically more indolent processes, like benign neoplasms, that may need no further intervention.
2. Patient age and clinical history can help to narrow the differential diagnosis.
Knowing the patient’s age and history provide important context when evaluating bone lesions.2 Many bone lesions preferentially affect specific age groups. Some benign lesions, such as unicameral bone cysts and fibrous dysplasia, are most commonly encountered in pediatric patients. In adults, metastatic malignancy and multiple myeloma become more common.
Knowledge of recent infection, history of similar lesions, degree and type of pain, and personal history of cancer can all be valuable in narrowing the differential diagnosis.
3. Lesion location is also helpful in determining the etiology.
Bone lesions often have a predilection for certain locations in the axial or appendicular skeleton.3 Lesions in the axial skeleton are usually more concerning for an aggressive process. Lesions in the appendicular skeleton can be characterized according to the transverse and longitudinal position within the bone. In long bones, a lesion may be in the epiphysis, metaphysis, or diaphysis. Several of the more common benign lesions are most often present in the metaphysis, such as enchondromas, while lesions in the diaphysis and epiphysis have a more limited differential. Most lesions are medullary-based, but some lesions are based in the cortex, including non-ossifying fibromas.
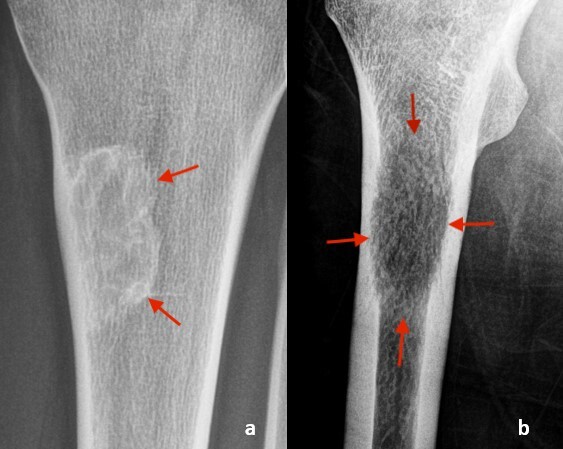
4. Lesions are typically divided into lucent, sclerotic, or mixed appearance.
The radiographic appearance of a bone lesion is based on the radiodensity of the lesion relative to the adjacent bone (Figure 1).4 Lucent lesions represent areas where bone is replaced or destroyed. In the setting of bone destruction, the lesion can be described as lytic. Sclerotic lesions are radiodense compared to surrounding bone and represent areas of increased bone formation. A mixed lesion has both lucent and sclerotic components, but one component may predominate.
5. For lucent lesions, the margins of the lesion and the effect on the cortex can help to differentiate aggressive from non-aggressive processes.
Lesion margination and cortical involvement are integral parts of radiographic assessment for aggressiveness (Figure 2).5 Geographic, well-defined, narrow margins without involvement of the cortex are non-aggressive features. In contrast, ill-defined, wide margins with erosion or destruction of the cortex suggest a more aggressive process and a higher chance of malignancy. Lesions with these aggressive features necessitate further investigation.
6. The presence and type of periosteal reaction can also help identify aggressive pathology.
Periosteal reaction is a response of the periosteum to an insult to the underlying bone (Figure 3).6 Solid periosteal reaction is seen in the setting of a slow-moving, indolent process, where the periosteum has time to develop smooth, organized bone. In contrast, a fast-moving, aggressive process does not allow for well-organized periosteal bone formation. This can result in periosteal reaction that appears lamellated (onion skin), perpendicular spiculated (hair-on-end), or divergent spiculated (sunburst), sometimes with a Codman’s triangle, all of which can be seen with aggressive processes like malignancy and infection.
7. Sclerotic lesions are less common than lucent lesions, with a narrower differential diagnosis.
The lower frequency of sclerotic lesions is due to fewer processes leading to an increase in bone formation.7 A bone island is a common isolated sclerotic lesion, while multiple sclerotic lesions raise concern for sclerotic metastatic disease, particularly from prostate or breast cancer. In younger patients, osteoid osteoma can present as a painful sclerotic lesion, while sclerotic osteosarcoma is usually accompanied by other aggressive features.
8. Multiple lesions are more likely due to metastasis or multiple myeloma, particularly in an adult.
While most primary bone tumors are solitary in presentation, multifocal bone lesions are suggestive of metastatic disease or multiple myeloma in adults. In the setting of suspected metastatic disease, a nuclear medicine bone scan can look for other lesions throughout the skeleton (Figure 4).8 For suspected multiple myeloma, serum protein electrophoresis can be obtained as the next diagnostic step. In children, multifocal lesions are more likely benign (e.g., fibrous dysplasia, enchondroma) and may be related to certain syndromes.
9. MRI, preferably with contrast enhancement, is the next best step for imaging lucent lesions that have any suspicious features.
MRI with intravenous contrast produces detailed images of bone lesions and the surrounding soft tissues (Figure 5).9 MRI can help differentiate benign cystic or fibrous lesions from aggressive lesions. For aggressive lesions, MRI can show the extent of marrow involvement and whether there is spread to the soft tissues, including blood vessels and nerves. The addition of IV contrast further aids in lesion characterization and assessing extent of disease.
10. Risk stratification and management decisions for bone lesions can be guided by the Bone-RADS system.
The Bone-Reporting and Data System (Bone-RADS) scoring system, developed by the American College of Radiology, provides a standardized framework for assessing and managing any potentially neoplastic bone lesions.10 The system categorizes a lesion by key radiographic and clinical features, such as periosteal reaction and endosteal erosion. This categorization allows lesion classification based on potential risk of malignancy, along with evidence-based recommendations on the next steps in patient care. Similar to the BI-RADS system in breast imaging, bone lesions can be scored as Bone-RADS 1 through 4, with 1 corresponding to a very low risk of malignancy and 4 to a high risk. Management recommendations range from no further evaluation to advanced imaging and orthopedic oncology referral based on the Bone-RADS score.




_are_shown_to_be_due_to_.jpg)
._coronal_.jpg)


_are_shown_to_be_due_to_.jpg)
._coronal_.jpg)