Introduction
We present the case of a patient with Becker Muscular Dystrophy with associated cardiomyopathy who was on a SGLT-2 inhibitor when he developed severe ketoacidosis following a brief illness with diarrhea and anorexia. This case highlights the difficulty of using SGLT-2 inhibitors in acute dehydrating illnesses as well as in patients with a predisposition to ketoacidosis.
Muscular Dystrophy is known to have the potential for ketoacidosis in the context of starvation due to impaired glycogen stores due to vastly reduced muscle mass.1
Guidelines established in the 2022 AHA report2 give a favorable recommendation to SGLT-2 inhibitors in Heart Failure with reduced Ejection Fraction (HFrEF), regardless of the presence of type 2 diabetes and without limitations for possible harmful effects. It is stated in the package inserts that these medications should not be used in type 1 Diabetes Mellitus; in Chronic Kidney Disease, Stage 4 or greater; or in patients with hypotension. Other medications in the guideline’s recommendation include angiotensin receptor/neprilysin inhibitor (ARNi) / Angiotensin Converting Enzyme inhibitor (ACEi), Beta-Blocker (BB), Mineralocorticoid Receptor Antagonist (MRA), SGLT-2 inhibitors, and diuretics as needed. Beta-blocker therapy is the only other class of medications for HFrEF that has a favorable recommendation without any recommendations that suggest harm. ACEi /ARNi have designation of potential harm in the case of angioedema history. MRA (Mineralocorticoid Receptor Antagonist) have designation of potential harm in the case of uncontrolled hyperkalemia. Both medications change their recommendation based on patient characteristics. Our case exposes some clinical conditions that could make the use of SGLT-2 inhibitors harmful.
Case Report
A 52-year-old man with a past history of Becker muscular dystrophy and systolic heart failure with an ejection fraction of 30% was admitted with a 2-day history of diarrhea, anorexia, and decreased urine output. He had a left ventricular ejection fraction of 35% by echocardiogram and had been placed on dapagliflozin 2 years prior. His current medications included carvedilol, furosemide, sacubitril-valsartan, dapagliflozin, cholecalciferol, and cetirizine.
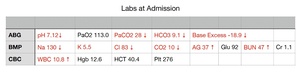
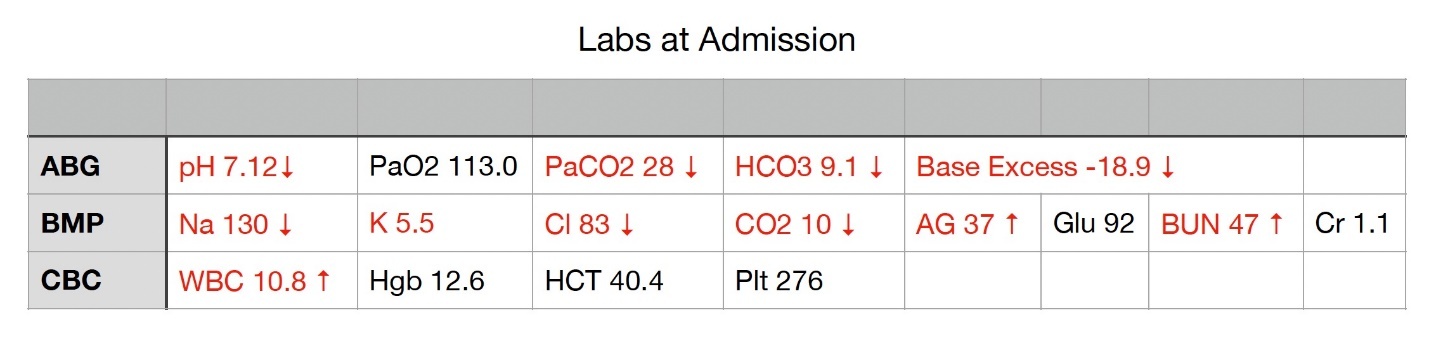
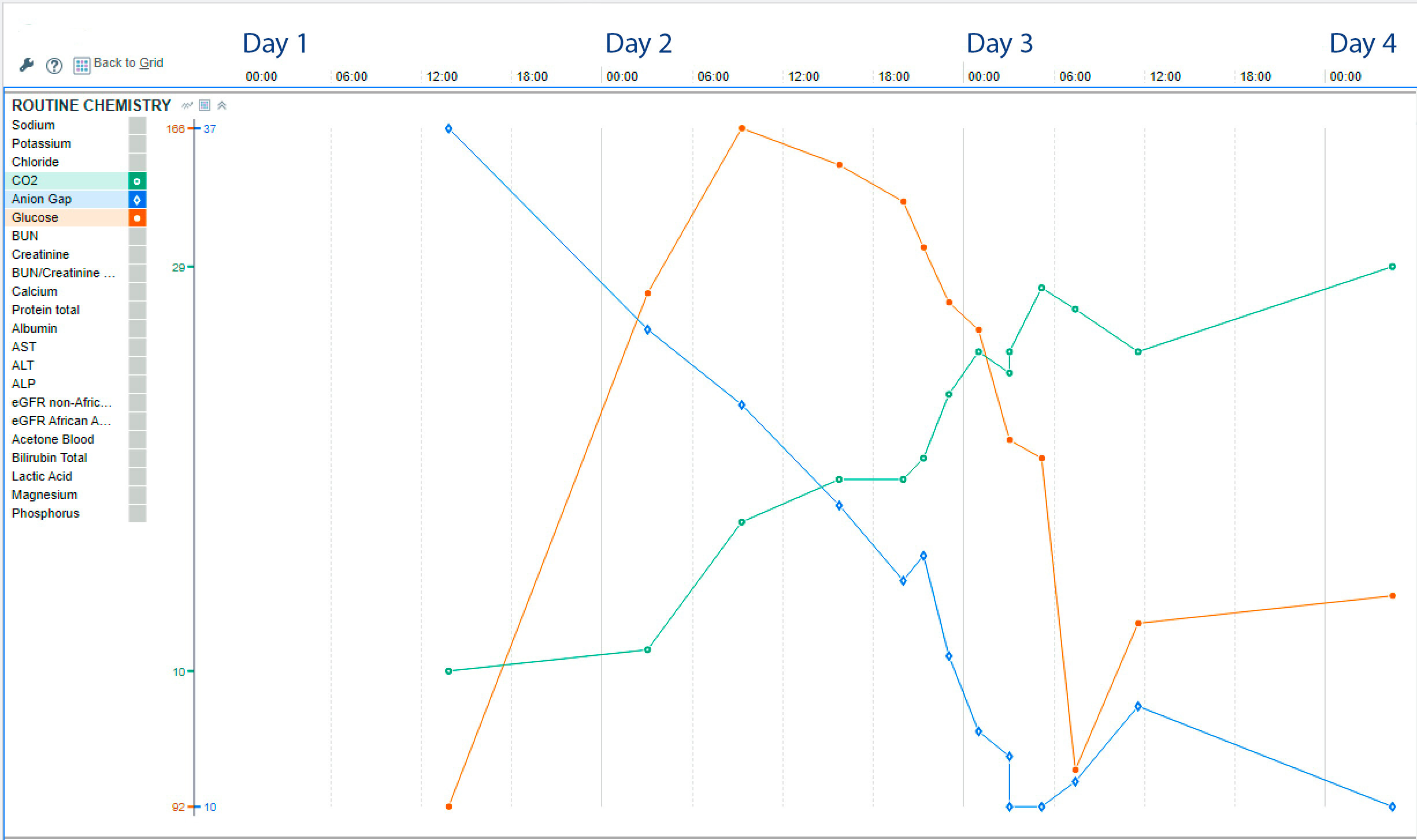
On initial presentation, he was hypotensive (59/32 mmHg), tachycardic (105 beats per minute), and tachypneic (18 breaths per minute) with temperature of 97.8° F. His Body Mass Index (BMI) was 25.1 kg/m2. He was acutely ill but had maintained cognition; his lungs were clear bilaterally; his cardiac exam revealed tachycardia with no gallop and warm lower extremities with no edema; he had muscular weakness consistent with BMD - bilateral foot drop, 2/5 strength in musculature in legs and 3-4/5 in his arms. A summary of labs at admission includes WBC was 10.8 K/uL, Hgb 12.6 g/dL, Na 130 mmol/L, K 5.5 mmol/L, CO2 10 mmol/L, Anion gap 37 mmol/L, BUN 47 mg/dL, Glucose 92 mg/dL, Cr 1.1 mg/dL (his baseline Cr was 0.1 mg/dL). ABG showed pH 7.12, PaCO2 28 mmHg, PaO2 113 mmHg, HCO3 9 mmol/L, Base excess -18.9 mmol/L (Figure 1, Labs at Admission).
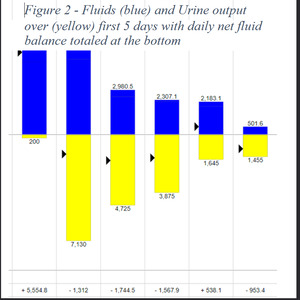
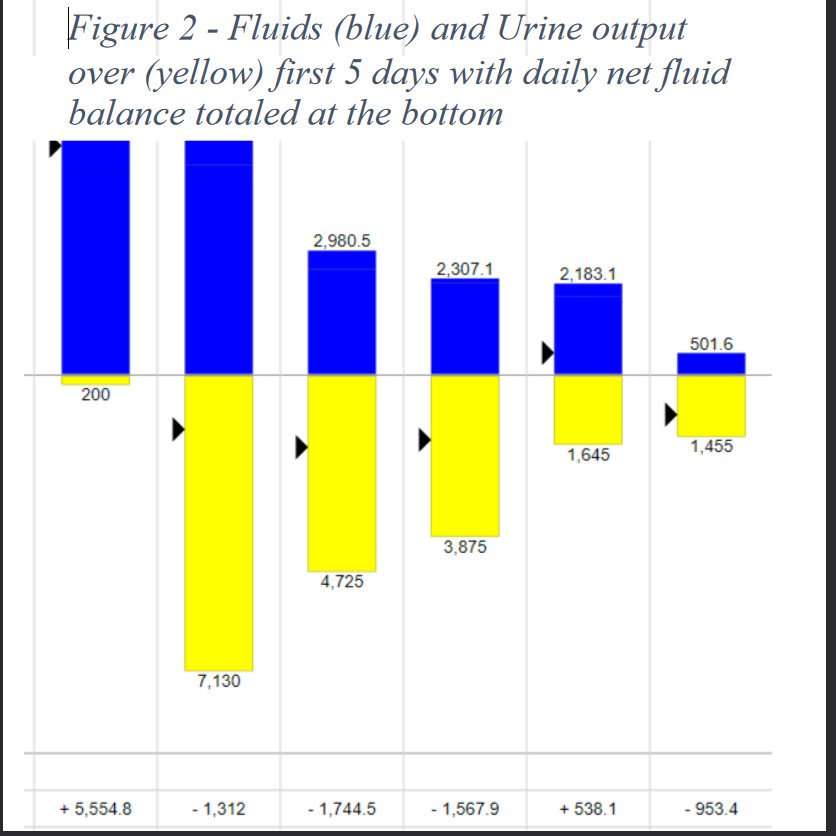
Urinalysis was not available due to anuria. Initial consideration included sepsis, and he received empiric antibiotics and fluid resuscitation - with 3 liters of isotonic fluid with no corresponding improvement in his BP and no pulmonary crackles or hypoxia. He was moved to the critical care unit for further fluids and norepinephrine infusion. Additional labs returned at this time showing lactate of 0.8 mmol/L, serum acetone LARGE (normal is negative), serum cortisol of 34 ug/dL, beta-hydroxybutyrate 130 mg/dL (normal range from 0 to 3), and HbA1c 4.7%. Over the course of the next 2 days, he continued to receive fluids as his anion gap normalized and he was weaned from norepinephrine. He received 10 liters of isotonic fluids in the first 2 days, and his urine output improved, then increased before normalizing. This graph of fluid balance is shown in Figure 2, with IV fluids in blue and Urine Output in yellow.
His first urinalysis returned 12 hours after presentation showing 3+ ketones and 3+ glucose. The best marker of his ketosis, beta-hydroxybutyrate, decreased from 130 to 20 over the first 2 days of treatment, still nearly 7 times the upper limit of normal. As his clinical condition returned to normal, further measurements of beta-hydroxybutyrate we not done, as the lab took several days to return.
He was placed on an insulin infusion after 12 hours of fluids, mostly isotonic but also with isotonic bicarbonate as well. His fluids were changed to dextrose-containing fluids to facilitate use of insulin infusion. Much of his management over the first 16 hours was empiric as his confirmatory labs were not available. Daily urinalysis was obtained to monitor the presence of ketosis – as his anion gap was affected by the use of bicarbonate-containing fluids. The insulin infusion was problematic and therefore intermittent because of hypoglycemic episodes. The insulin infusion was finally stopped when there was no further evidence of urinary ketones. The insulin infusion had to be restarted with the return of ketonuria. Ultimately, after 10 days from his most recent dose of dapagliflozin, the patient had a series of two negative urinalyses for ketones, and the insulin infusion was able to be discontinued. At this point, his clinical condition improved. He was ultimately discharged home with discontinuation of dapagliflozin.
Discussion
SGLT-2 inhibitors are used in the treatment of type 2 diabetes mellitus and systolic heart failure. The mechanism of action of SGLT-2 inhibitors involves decreasing reabsorption of the filtered glucose load in the urine at the proximal convoluted tubule, thereby increasing glucose in the urine and facilitating an osmotic diuresis.3 This effect lowers the plasma glucose which then reflexively lowers the insulin level. There is a ketogenic tendency with the use of SGLT-2 inhibitors, and the proposed mechanism for this tendency is a lowering of the insulin level that results from lower plasma glucose.4 Insulin has an antilipolytic property that prevents ketosis, and it is proposed that the lowering of the insulin level by treatment with SGLT-2 inhibitors increases lipolysis in adipose tissue, leading to ketosis.5
Becker Muscular Dystrophy4 is a form of muscular dystrophy resulting in progressive muscle degeneration. It is an X-linked recessive disorder, thus primarily affective to males. Becker Muscular Dystrophy affects the proximal muscles of the lower limbs and, later in the course of the disease, can affect cardiac muscle, resulting in cardiomyopathy. The disease generally has clinical manifestations of leg weakness in adolescence. Some patients retain the ability to walk into adulthood. For the purposes of our discussion, Becker Muscular Dystrophy results in destruction of skeletal muscle mass.
Euglycemic DKA6 is a rare complication of diabetes. It is typically seen in conditions in a diabetic patient that result in an imbalance between insulin and counter-regulatory hormones leading to the use of ketones. These conditions are typically fasting, surgery, and pregnancy. The new addition to this list is the use of SGLT-2 inhibitors in the general treatment of diabetes. Euglycemic DKA is rarely seen in patients without diabetes, but there have been reports of the disease in heart failure patients treated with SGLT-2 inhibitors,7 one of which had muscular dystrophy.
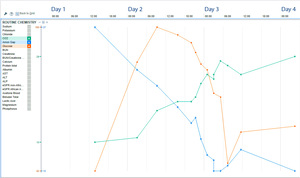
Our patient had been taking dapagliflozin for the treatment of systolic heart failure, in accordance with the recently released guidelines. After starting the medication, he was seen for an annual wellness visit, where a urinalysis was normal with the exception of >1000 glucose - consistent with the effect of dapagliflozin. His emergency visit was preceded by 2 days of diarrhea and 1 day of anorexia, which can lead to ketosis in muscular dystrophy. On arrival at the hospital, he was hypotensive with labs consistent with ketoacidosis and acute renal failure. He was treated with dextrose containing fluids, insulin infusion, and vasopressors, and his metabolic derangements resolved over the course of 3 days (Figure 3), though his serum ketones remained elevated.
His case, though complicated by his muscular dystrophy, reveals a difficult scenario that can be present, to a lesser degree, in other patients. Our patient has very limited ability to withstand fasting or a prolonged dehydrating illness given his propensity to ketone formation because of limited glycogen stores. His reduced muscle mass, evidenced by his Becker Muscular Dystrophy and very low baseline Cr of 0.1 mg/, offers little to no reserve glycogen in the instance of a prolonged fasting state. As glycogen stores in the liver are depleted, there are generally reserves in muscle glycogen; without these reserves, ketone formation is necessary. It is well documented that the mechanism of action for dapagliflozin is forced glucosuria and natriuresis with subsequent osmotic diuresis. The resultant decreased blood glucose then reduces the body’s insulin production by BETA cells in the pancreas and increased glucagon secretion by the ALPHA cells in the pancreas. This effect favors breaking down glycogen stores to access glucose and ketones rather than using available glucose, thus rendering ketone formation a process that is more readily available in those using SGLT-2 inhibitors. Patients with reduced muscle mass, like our patient with muscular dystrophy, have relatively small glycogen stores (predominantly in skeletal muscle) – thus a greater tendency to use ketones in periods of fasting. This idea seems to imply that there may be a subset of patients with systolic heart failure for whom this mechanism of diuresis could present an opportunistic risk of danger. These patients could potentially be a combination of thin, elderly patients with reduced muscle mass. There should be a recognition of the potential harm related to the use of SGLT-2 inhibitors.
The AHA / ACC / HFSA guidelines that were published in 2022 reference different management options of systolic heart failure.2 The four pharmaceutical options referenced are beta-blockers, ACEi / ARB (Angiotensin Receptor Blocker) / ARNi , MRA, and SGLT-2 inhibitors. Each drug class is given a class of recommendation, ranging from 1 (benefit) to 3 (harm) based on a particular level of evidence, ranging from A (high-quality / Randomized Controlled Trials) to C (meta-analysis or expert opinion).
The Class 3, Harmful, designations in the recommended treatment for heart failure include the following:
-
Avoid concomitant use of ARNi within 36 hours of the use of ACEi
-
Avoid use of ACEi or ARNi with a history of angioedema.
-
Avoid use of MRA in patients with hyperkalemia.
There are no listed Class 3, Harmful, designations for SGLT-2 inhibitors.
Our case presents a reason for pause in the prescribing of SGLT-2 inhibitors for the treatment of systolic heart failure, namely a history of ketosis. Furthermore, with the coming ubiquity of this class of medications - diabetes mellitus type 2, heart failure with reduced ejection fraction, and heart failure with preserved ejection fraction - the prescriber will need to be cautious in the selection of patients to receive this medication, as there are patients like the one presented who will tolerate the known side effects of SGLT-2 inhibitors poorly. This report should give pause to the prescriber of dapagliflozin to consider the risks of harm.