Case Presentation
A 10-year-old presented with a six-week history of a slowly enlarging, pruritic annular patch initially thought to represent granuloma annulare. The condition failed to respond to a combination of triamcinolone acetonide 0.1% cream and clotrimazole 1% cream twice daily. There was no history of tinea pedis. She did participate in competitive youth sports. Physical examination revealed a solitary oval 20 cm x 18 cm erythematous scaling patch with central clearing on the left anteromedial calf (Image 1a, 1b).
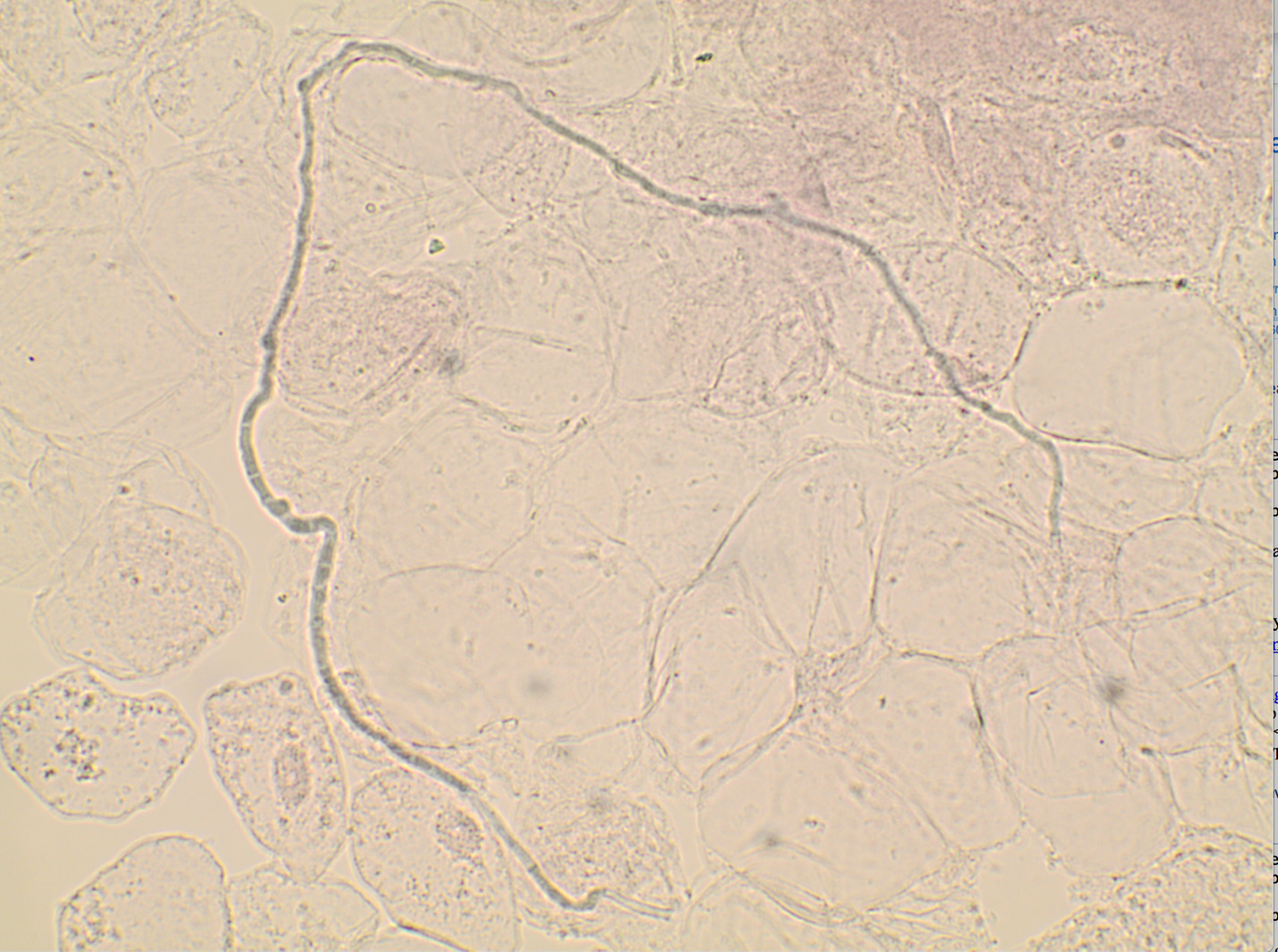
Tinea corporis was suspected. A potassium hydroxide preparation from the advancing, scaled border of the patch demonstrated septate hyphae confirming the diagnosis of tinea corporis (Image 2). The previous topical treatments were discontinued, and ketoconazole 2% cream was applied twice daily for one month. Excellent clearing was noted. The ketoconazole 2% cream was continued once weekly for 6 weeks to ensure the condition did not recur.
Discussion
Tinea corporis, a common fungal infection with a lifetime risk of 10-20%, is primarily caused by Trichophyton rubrum, Trichophyton tonsurans, and Microsporum canis, often affecting children and young adults.1,2 It classically presents as an erythematous, annular, pruritic patch with central clearing and well-defined active border with leading scale.3 Pustules or vesicles may be present in some cases. The lesions vary in size and number, with larger lesions potentially coalescing into polycyclic patches.2 Risk factors include personal history of dermatophytosis, contact with affected family members, pets, crowded living quarters, recreational exposure, immunosuppression, and diabetes mellitus.2 It is important to always consider the differential diagnosis of annular rashes with special attention to distinguishing features (Table 1).
In this case, the diagnosis was straightforward: a slowly expanding erythematous scaled patch with central clearing. “Shotgun treatment” with combination topical steroids and topical antifungals is often ineffective. Lowering local immunity with topical steroids can lead to treatment failure and fungal resistance even when using concomitant topical anti-fungals.4 Furthermore, topical steroid use can produce “tinea incognito” where decreased scaling and erythema obscure the classic clinical features leading to misdiagnosis or delayed diagnosis.
When tinea is suspected, superficial skin “scraping” with a rounded #15 or #10 blade or curette will produce scale for immediate examination with KOH 10% solution or inked KOH solution (Chicago Blue or chlorazole black E).5 The more scale obtained, the higher is the likelihood of identifying hyphal elements when present. The presence of septate hyphae confirms the diagnosis (Image 2).1 When materials for a KOH are unavailable, scale can be submitted in a clean container for polymerase chain reaction (PCR) which can be resulted in several days or a fungal culture which takes 3-4 weeks. False negatives may occur. If a strong concern for tinea exists, a PCR or fungal culture should still be obtained. In contrast to topical steroids, empiric therapy with antifungals may be used while awaiting confirmation, as it would be unlikely aggravate other dermatoses.
Topical antifungals, such as fungistatic azoles and fungicidal allylamines, are utilized initially in the treatment of tinea corporis with oral medications reserved for widespread or treatment-resistant cases.2 Prevention of recurrence is accomplished by 1) treatment of concomitant tinea pedis when present and 2) avoidance of exposure to environments that could lead to re-infection, such as fomites that spread infection from other athletes.
Primary care physicians should be aware of important diagnostic features and effective management approaches to correctly diagnosis tinea prior to treatment.6
Acknowledgements
One author has participated in multi-center clinical trials with: Corevitas (Formerly Corrona) Psoriasis Registry, Sanofy and Novartis. Stock: Veradermics, Inc. All other authors have no conflicts of interest.