Introduction
This case report showcases the presentation, work-up, diagnosis, and treatment of a rare extra-abdominal leiomyosarcoma. This case is unique as a majority of leiomyosarcoma tumors are found in the abdominal cavity, with extra-abdominal leiomyosarcomas making up only 10% of leiomyosarcomas.1 In addition, we discuss etiology, genetic predispositions, and tumor surveillance of leiomyosarcomas.
Patient Information
A 48-year-old African American male with past medical history of asthma, hypertension, dyslipidemia, Non-Alcoholic Fatty Liver Disease, glucose intolerance, solitary testicle, obstructive sleep apnea, contact dermatitis, vitamin D deficiency, and obesity presented with a chief complaint of a left thigh mass of nine months duration.
The patient states that his left thigh mass has increased (especially in the last one month) and denied any tenderness, pruritus, ulceration, or discharge/bleeding from the thigh lesion. He describes the left thigh swelling as sudden in onset, progressively increasing in size, localized to the anterior aspect of the left-upper thigh, and not associated with any known trauma or falls. Patient denies any use of cigarettes and drinks alcohol socially.
Clinical Findings
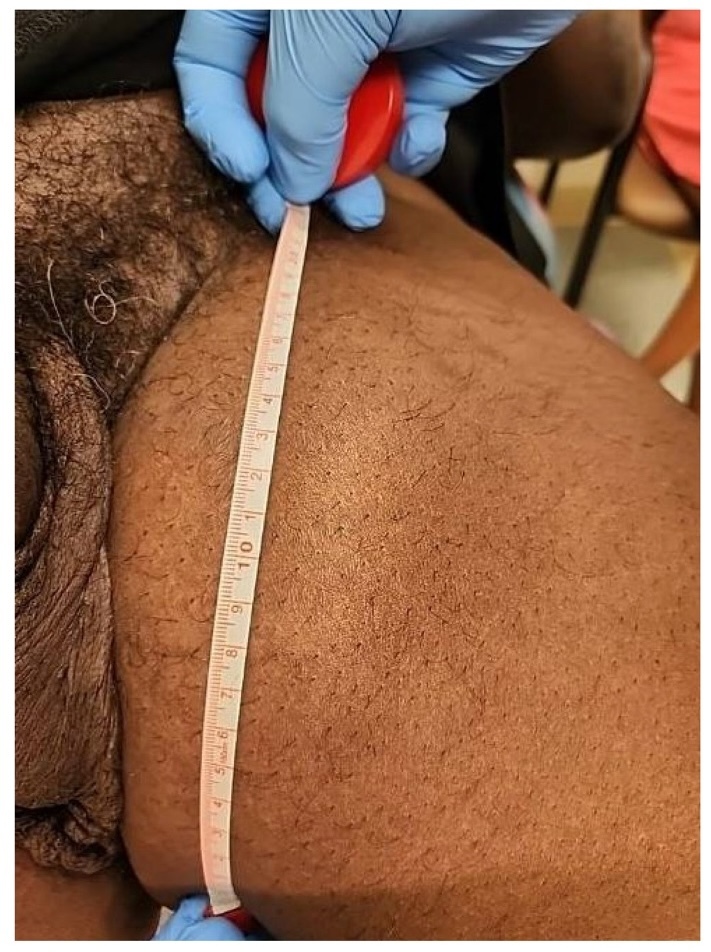
On physical examination, he had an elevated blood pressure (BP) reading of 148/88 mmHg, and a body mass index (BMI) of 40.9. He also had a 6x7 cm left thigh mass (Figure 1) which was soft, mobile, non-tender, non-erythematous, and non-ulcerated.
Diagnostic Assessment
Patient underwent an ultrasound (USS) of the left thigh mass which demonstrated a 7.5-cm well-circumscribed hypoechoic mass with irregular border and internal doppler flow. As malignancy could not be excluded, further assessment with a Computed Tomography (CT) scan of the left thigh and excisional biopsy were undertaken.
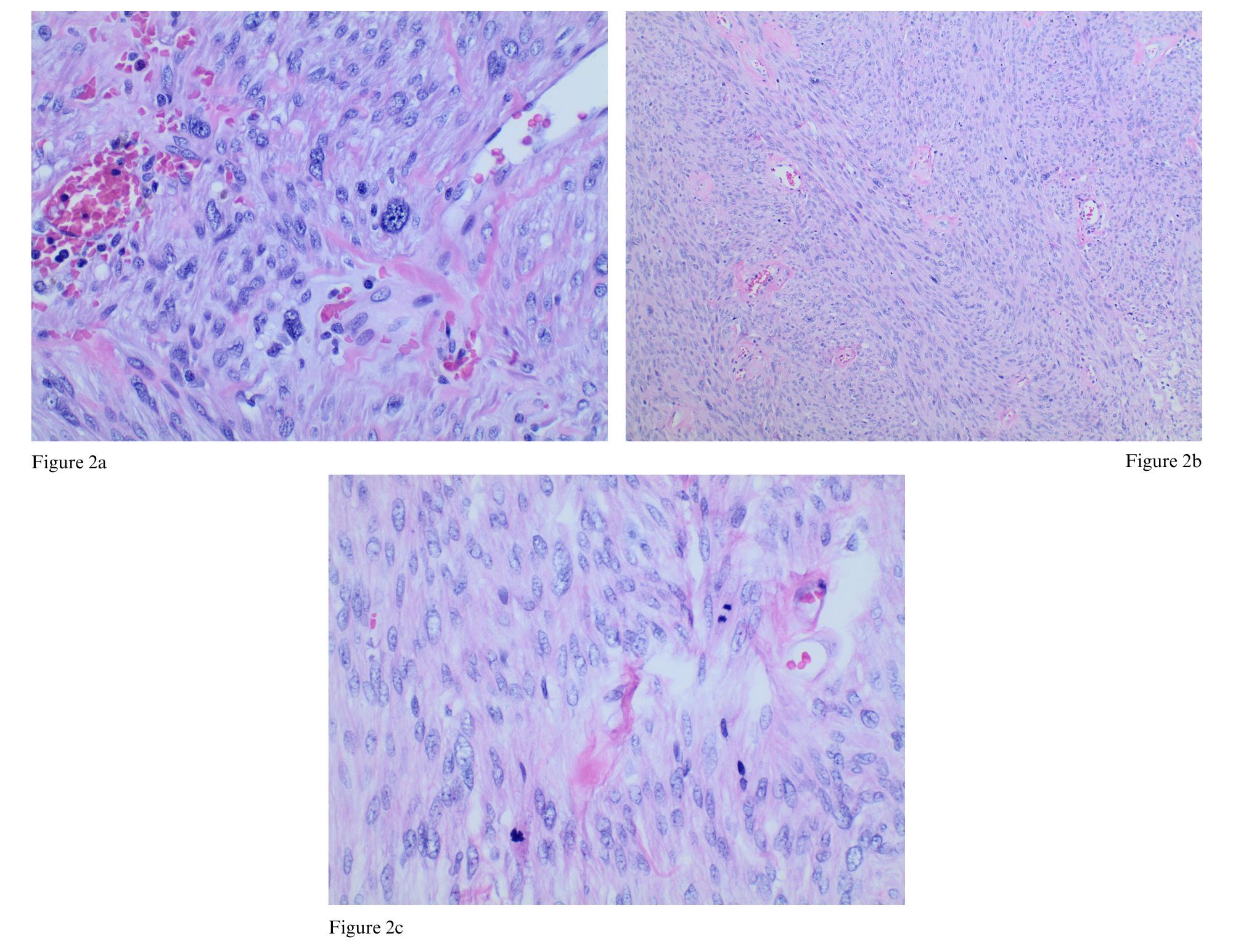
The CT of the left thigh demonstrated a 6.5-cm soft tissue mass in the left inguinal region with subcutaneous soft tissues, reflecting a nodal mass or other soft tissue neoplasm. A subsequent Interventional Radiology (IR)-guided biopsy showed histopathology consistent with atypical smooth muscle tumor proliferation with foci of significant cytologic atypia and rare mitotic figures (Figure 2) consistent with leiomyosarcoma.
A metastatic work-up was negative for metastatic lesions in the chest and showed a 6.5-cm heterogeneously enhancing mass in the left inguinal region, consistent with the biopsy-proven leiomyosarcoma, and mildly enlarged bilateral inguinal lymph nodes on Magnetic Resonance Imaging (MRI) pelvis with and without contrast (Figure 3).
Therapeutic Intervention
The patient was seen by Surgical Oncology and underwent a radical resection of left thigh sub-fascial mass measuring 10.5 x 9.5 x 4.0 cm, achieving an R0 negative resection margin. His staging was T2Nx, grade 2/3. He is currently undergoing external beam radiation therapy.
Follow-Up and Outcomes
The patient is tolerating radiation therapy well with Radiation Oncology. He has met with Medical Oncology who recommended adjuvant chemotherapy. Surgical Oncology plans to place a chemoport and ordered repeat surveillance imaging.
Discussion
Leiomyosarcomas (LMS) are tumors derived from smooth muscle, and make up approximately 15-20% of newly diagnosed soft-tissue tumors in adults, and with a peak incidence at 70 years of age.1,2 Extra-abdominal LMSs, such as our case patient’s, make up less than 10% of LMS cases.1 Metastases are common in LMS, with the most frequent sites being lung and liver. Surgical excision is the curative treatment for LMS, with adjuvant chemotherapy providing reduced risk for recurrence.
Though leiomyosarcomas often develop as a result of de novo mutations, genetic predispositions associated with LMS include retinoblastoma, Li-Fraumeni Syndrome, and unbalanced karyotypic defects.2 In addition, environmental exposures may pose an additional risk for LMS. Several case reports have explored post-radiation leiomyosarcomas, highlighting this risk factor.3–5
This patient’s enlarging thigh mass is a common presentation of extra-abdominal leiomyosarcomas. Clinical presentations of other subtypes of LMS may include venous thromboembolism or nonspecific symptoms caused by displacement of structures in the area of involvement, such as hemoptysis in cases with lung involvement.2
Tumor detection via imaging is done in a stepwise approach. In extra-abdominal LMS, USS is a common first imaging modality and aids in ruling out other disease processes. USS of LMS often shows a hypoechoic mass with increased vascularity.6 Positive USS prompts clinicians to further evaluate suspicious masses; CT of lesion is an appropriate next imaging step in diagnosis, followed by biopsy. CT chest should be conducted after diagnosis to assess for lung involvement.
Leiomyosarcoma carries a high risk of metastases and recurrence. The Memorial Sloan Kettering Cancer Center Nomogram is used to approximate rate of recurrence and should be calculated post-operatively.7 The patient described above carries a MSKCC Nomogram of 28-38%, reflective of a high risk of recurrence. Cross sectional imaging is recommended every 4 months for 2 years post-operative, every 6 months 2-5 years post-operative, and annually after 5 years.8
Conclusion
Primary care physicians serve a vital role in diagnosis and require high clinical suspicion to diagnose rare tumors such as leiomyosarcomas. Patients with similar signs and symptoms as those discussed in our case patient should be evaluated with imaging to include initial ultrasound followed by axial imaging with CT or MRI. We advocate for referral to specialized surgical providers who are experts in the management of sarcomas to include surgical oncologist or orthopedic oncologist. We also advocate for discussion of all available options to include surgical resection, neoadjuvant or adjuvant radiation therapy, and neoadjuvant or adjuvant chemotherapy.
Informed Consent
Informed consent for this case report was obtained from the patient.



_and_axial_(3b)_views_signific.jpg)
_and_axial_(3b)_views_signific.jpg)